Entries in care collaboration (11)
Central Indiana Beacon Community’s Pilots Leverage Remote Monitoring Technologies to Successfully Engage Patients
 January 9, 2013
January 9, 2013 ![]()
Mass General’s Ambulatory Practice of the Future Engages Patients through Shared Decision Making
 October 24, 2012
October 24, 2012 
More than two years ago, Mass General launched their Ambulatory Practice of the Future, an innovative primary care clinic for employees and adult dependents. Developed as a Patient-Centered Medical home and ACO, today they support 3,000 enrolled patients with three doctors and two nurse practitioners.
This innovative practice was designed for and with patients for a better patient experience. Their experience begins with the initial greeting and extends through ongoing care interactions. There is a strong focus on patient education and empowerment. The care team collaborates to support each patient both in person and online. One of the goals of the practice is to reach patients where they are both physically and with their health.
Designed to Support Shared Decision Making
Once patients enter the welcoming and intimate care setting at The Ambulatory Practice of the Future (APF), they are ready to collaborate with their clinician. Sitting side by side, they review the medical record together and begin the discussion with health goals.
“We actually added a data field to the record called ‘Health and Life Balance Plan’ where we document mutually agreed upon goal(s) for the coming weeks and months and then it is easily reviewed by the patient via their portal after the visit and in preparation for upcoming follow- up encounters”, explains Dr David Judge, Medical Director, Ambulatory Practice of the Future, Massachusetts General Hospital.
This collaborative approach has helped patients who have not historically been able to get engaged around a goal. Dr Judge shares a story about a 54 year old woman with diabetes who was reluctant to discuss next steps in management due to her fear of taking insulin. After allowing her to shape the goals with a focus on other areas of lifestyle management initially, coaching to realize some success and encouraging patience with the process, she has recently decided to proceed with insulin therapy.
Patient Engagement Tools
APF uses shared decision making videos developed by the Foundation for Informed Medical Decision Making to educate patients about screening tests and in managing specific medical issues such as prostate cancer.
Between their visits, patients can access the portal to view their medical information and communicate securely with their clinician. Although the care team can access the EMR from their mobile devices, APF expects that patients will be able to access their portal and records via mobile devices in the near future.
Patients can currently participate in an online visit with their care team. Dr Judge describes one of the complex patients that they monitor closely with frequent virtual visits. “Mr. K is struggling with end stage renal failure, congestive heart failure and it has become difficult for him to come for office visits. Between scheduled virtual visits, emails from the patient and his wife and monitoring by visiting RNs, we are able to manage his needs fairly well with rare office visits. We are on the verge of implementing true remote monitoring technologies but currently the patient or RN need to report the measures (i.e. blood pressure, weight, blood sugar, PHQ 9 depression score, etc.).”
On the prevention side, several employees are using mobile apps to track their daily lifestyle choices regarding exercise and nutrition and sharing the information with their clinicians during their visits.
Future Path to Patient Engagement
During my panel at the recent Shared Decision Making Conference, Dr Judge spoke about some exciting new ways APF will be leveraging technology to engage their patients.
“We will be piloting the concept of 'apprenticeship' in which patients go through a more formal education process with coaching and demonstration of increased knowledge and skill to push the boundary on self management. We are developing programs tailored to specific medical conditions (i.e. HTN, DM and Depression). Goal setting for each patient helps the team to understand how to customize the program and to identify what specific barriers may be preventing success.”
“As we have done with diabetes, we expect that patients will learn not only to change their lifestyle and make healthier choices but also adjust medication in the management of multiple chronic diseases. The care team will be able to monitor and assist but patients will truly drive their own care more effectively from day to day”, adds Dr Judge.
APF is starting a pilot soon using a mobile tablet that “allows very easy synchronous communication to transmit monitored blood pressure and to enable the patient and team to collaborate around lifestyle management and medication adjustment”.
The term “apprenticeship” is being used by Dr. John Moore at MIT Media Lab. Dr Judge explains, “I think it appropriately describes the next step in the evolution of making shared decisions with patients. Beyond that is potentially a mastery of health and the potential for patient - to - patient support to grow. We are hoping to launch both face- to -face and virtual peer to peer interactions in the near future.”
 care collaboration,
care collaboration,  educating consumers about health and wellness,
educating consumers about health and wellness,  self- management health tools in
self- management health tools in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Centered Medical Home,
Patient Centered Medical Home,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Portal,
Patient Portal,  Personalization eHealth,
Personalization eHealth,  shared decision making ehealth
shared decision making ehealth Group Health‘s Mobile App Brings Consumers and Clinicians Closer for Collaboration and Convenience
 May 14, 2012
May 14, 2012  In early 2011, Group Health set out to find ways to use mobile to help members manage their health and make better decisions about where, how and when to get care. “We view mobile as another channel of delivering patient care which is important to us given our mission of serving the greatest number of people”, explains Colby Voorhees, Senior Product Manager at Group Health.
In early 2011, Group Health set out to find ways to use mobile to help members manage their health and make better decisions about where, how and when to get care. “We view mobile as another channel of delivering patient care which is important to us given our mission of serving the greatest number of people”, explains Colby Voorhees, Senior Product Manager at Group Health.
Group Health launched their award winning mobile application with key capabilities such as care management with “My Care”, care guidance with “Consulting Nurse” and care planning with “Wait Times” for Pharmacy and Laboratory services.
Group Health’s app moves beyond the mobile capabilities enabled by other health plans which let consumers look up health information, check symptoms or find urgent care.
“We’ve received very positive feedback from members on our version 1.0 app but were surprised that members expected our mobile application to have more capabilities out of the gate such as refilling a prescription or accessing information on the entire family”, Colby reports.
“Love the new app but am frustrated that I have to go to the full site to reorder meds. Will this be available on the new app soon?”
“Please provide a Parental Access feature in the next update, soon. I have to take my kids in much more than I go in so most of the time I end up using a web version on my phone (not fun) instead of the app.”
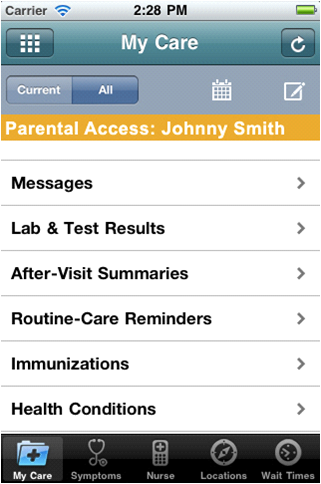 Last summer, Group Health released their 1.5 version with prescription refill and parental access capabilities. Their mobile app now has over 36K downloads (iPhone 25+K) and Android 11+K) by 14% of their web access users and 5% of their total members.
Last summer, Group Health released their 1.5 version with prescription refill and parental access capabilities. Their mobile app now has over 36K downloads (iPhone 25+K) and Android 11+K) by 14% of their web access users and 5% of their total members.
The two most used mobile app features are “My Care” (37%) and “Wait Times” (36%) followed by “Symptom Checker” a distant third (10%).
In “My Care”, consumers can now see their personalized list of care reminders for preventive and chronic conditions (if applicable), communicate with their clinicians (e.g. primary care and specialists), review their ‘after visit summary’, refill a prescription and access care information for children under twelve such as immunization timing. Members can also use the scheduling feature to check available appointments and book them with their PCPs. “It’s like picking a seat on the plane that you want instead of having someone else select it for you”, exclaims Colby.
Within “My Care”, the top three features used are Reading Messages (32%), Viewing Lab Results (25%) and Making Future Appointments (16%).
Group Health’s Mobile Motivation
The product team at Group Health remains focused on taking complex tasks that the consumer is trying to do and making them simple. Group Health collaborates with consumers to get input on mobile concepts and works closely with them through usability research to make sure the capabilities meet expectations and the interface is intuitive.
While Colby discussed their mobile research, I heard members voice their desire for increased convenience and an improved customer experience.
“If they had an app that made it that easy to interact with healthcare, I would choose Group Health.”
"My spouse would absolutely download that app to take care of his health since he can use it while commuting to work on the bus or while he is waiting in line.”
“I absolutely appreciate the forward thinking technological advances that Group Health has. Something seemingly as simple as an iPhone app to access my health records, completely changes and improves my experience in a way that other knuckle dragging change adverse medical providers just can't comprehend. Thank you.”
What is next for Group Health on the mobile front? Colby reminded me that they are only on their 1.5 mobile app version and there are opportunities ahead such pushing communications to consumers instead of relying on them to access their My Care dashboard.
As an integrated care system, Group Health has the advantage of leveraging their common platform for patients and providers to support care collaboration and self- management. Consumers can use mobile to access a single source for their care communication and transactional needs.
“We are thinking about the continuity of the care interaction with the clinician. There is a big divide between phone calls and in person visits. We already have secure messaging and can see where video might be the opportunity to bridge the gap in a low cost and high convenience way for patients and providers” shares Colby.
Within healthcare, the consumer demand for mobile services is quickly outpacing the apps being supplied by organizations. Consumers want all the features available on their specific mobile device, which poses a big challenge to organizations that don’t have the resources to fund all of the mobile platforms. The key will be to identify, prioritize and deliver the most meaningful features which will enhance the member experience, enable care collaboration and empower consumers to simply engage in their health.
Shared Decision Making Tools Engage Consumers for Better Outcomes and a Better Experience
 September 27, 2011
September 27, 2011 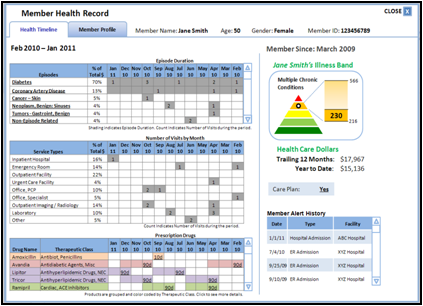 CareFirst BCBS Medical Home SDM Tool
CareFirst BCBS Medical Home SDM Tool
Over two years ago, I led a panel on patient decision support tools for a large interested crowd in Boston, despite the very snowy day.
Since then, I have noticed a few key changes. Physicians are now prescribing information to patients, using the EMR to send emails with links to health resources. And innovative health plans are playing a role in bringing shared decision making tools to engage and empower their members. Health Plans have a big cost saving incentive when these tools educate their members about less invasive and less expensive options.
3 Key Engagement Drivers With Shared Decision Making Tools
While evaluating technologies for my panel on “Evolving Web & Mobile Tools to Engage Consumers in the Shared Decision Process”, I identified how three key drivers of consumer engagement are being utilized:
1. Education
These tools show the consumer what the treatment entails and share patient stories which tell them what to expect. This education reduces anxiety by putting the consumer in control to understand their health issues and presenting options to address them.
2. Evaluation
Shared Decision Making tools are ideally designed for “preference sensitive conditions” where there are multiple clinical options (For information about target conditions, see the recent report on the Dartmouth Atlas Project which was developed with The Foundation for Informed Medical Decision Making). The most effective tools offer alternatives, capture preferences and guide the consumer through the process while documenting their decisions. This helps set expectations for their experience and supports the discussion with their doctor or care coach.
3. Collaboration
As the patient and clinician/coach review the SDM summary document together, they can discuss questions, concerns and comments to make the best decision.
Health Plans Leverage Shared Decision Tools
During the panel, health plans described using Shared Decision Making tools to engage members in two key areas:
- Medical Home
Panelist Zev Lavon, PHD, Director Solution Architecture, CareFirst BCBS emphasized “the story of the patient is not their last doc visit or lab test”. CareFirst launched their Primary Care Medical Home initiative across a panel of physicians deploying communication tools to push information to patients to support the management of their chronic conditions.
-
Wellness Coaching
According to Mark L. Robitaille, MBA, Head of Care Management Support & Engagement, Aetna puts these tools into the hands of their health coaches to send emails with resources links to members or use the tools to look up information for the members without internet access.
Independent Health panelist, James J. Mis, MBA, Communications Manager, Health Care Services, described their interactive voice response campaign to inform members about viewing a shared decision making video (from Emmi Solutions) selected for their specific health interest.
Emerging Mobile SDM Tools
With a high penetration of smart phones and strong usage across minorities, health care organizations are realizing the tremendous opportunity to deploy mobile applications to engage consumers. To date, most health mobile health applications have been focused on wellness with educational information and tracking.
Panelist Changrong Ji, Senior Solutions Architect, CareFirst BCBS described the opportunity for mobile shared decision making tools. In the future, she envisions that sensors will capture the context of the consumer’s daily life, database analytics will identify patterns and machine learning will be used to help identify relevant mobile messages to send back to the consumer.
Healthwise’s View on Patient Response
During the Shared Decision Making Summit, the chairperson, Don Kemper, Healthwise’s CEO discussed the opportunity for shared decision making tools to give a “voice to the patient”. After the physician prescribes health information, the tool gathers patient’s preferences to document them in the medical record. I strongly agree with Don as he explains “there is no better way to engage the patient than to assure them that their voice will be heard in treatment and care plan decisions”.
Shared Decision Making Tools for Your Consumers
What are you doing to bring Shared Decision Making Tools to your consumers to motivate engagement in their health and wellness? I can help guide you through the process of identifing, evaluating and piloting these technologies to deliver better outcomes and a better experience for your consumers.
Evolving Web Based and Mobile Tools to Engage Consumers in the Shared Decision Making Process
 September 6, 2011
September 6, 2011

World Congress Leadership Summit on Shared Decision Making
September 23, 2011
Panel Session:
Moderator:
Sherri Dorfman, MBA, Chief Executive Officer, Stepping Stone Partners
Panelists:
- Mark L. Robitaille, MBA, Head of Care Management Support & Engagement, Aetna
- Changrong Ji, Senior Solutions Architect, CareFirst BCBS (Mobile strategy)
- Zev Lavon, PHD, Director Solution Architecture, CareFirst BCBS (Web strategy)
- James J. Mis, MBA, Communications Manager, Health Care Services, Independent Health
 care collaboration,
care collaboration,  mobile health and wellness texting,
mobile health and wellness texting,  online health and wellness coaching,
online health and wellness coaching,  patient centered medical home,
patient centered medical home,  personalization for health and wellness in
personalization for health and wellness in  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Decision Support,
Patient Decision Support,  Personalization eHealth,
Personalization eHealth,  shared decision making ehealth
shared decision making ehealth