Entries in patient ehealth engagement (13)
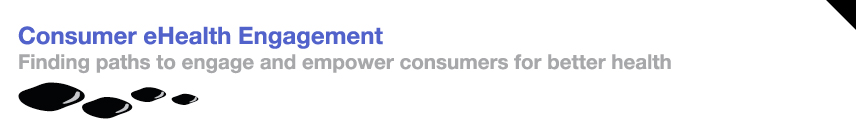
Geisinger Drives Mobile Patient Engagement with Education through iBooks & iTunes University
 August 1, 2016
August 1, 2016 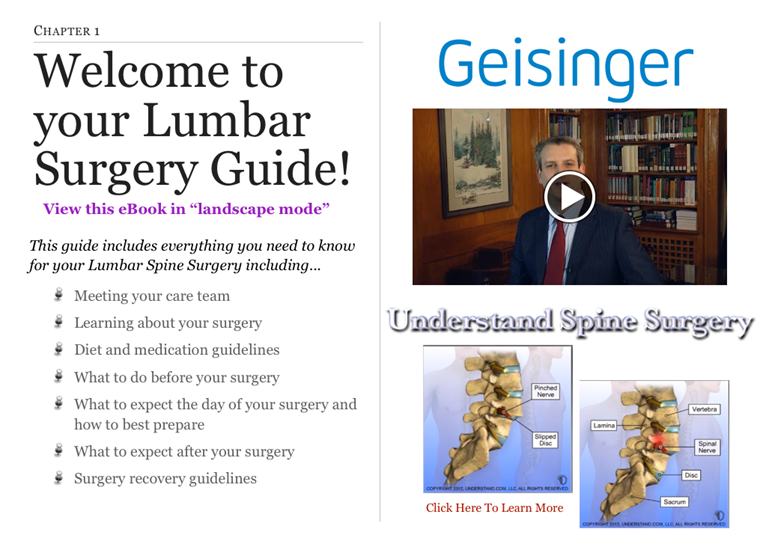 With the shift to value- based care, health systems are investing in mobile technologies to increase patient engagement and care quality while reducing the cost of care delivery.
With the shift to value- based care, health systems are investing in mobile technologies to increase patient engagement and care quality while reducing the cost of care delivery.
Geisinger, an award winning healthcare system based in the Mid-Atlantic with 12 hospitals and a 510K+ health plan, is a leader in patient engagement. Within their organization, the Geisinger in Motion team focuses on strategic initiatives to drive patient engagement by co-creating with patients on digital technology solution design, capabilities and efficacy.
Geisinger’s digital patient engagement initiatives are designed to support three key strategies 1) “understand my health”, 2) “manage my stay or visit” and 3) “control my condition (or specific acute episode)”.
Last fall, the Geisinger in Motion team embarked on a project to enhance their patient education resources, which spans all three patient engagement strategies. Although they already offered a comprehensive set of patient education materials (i.e. handouts, online resources, targeted classes, individual conversations), Geisinger was looking to expand the reach of these resources for patients and their families.
“The genesis of the idea came from a pilot for patients that were having Lumbar Spine surgery”, explains Chanin Wendling, AVP, Geisinger in Motion. Geisinger focused on this patient population because of the prevalence back pain problems across the nation, the volume of surgeries done annually (approximately 2,000) and high patient co-pays for the surgery.
“For this pilot, we loaded 10 iPads with educational content and loaned them to patients for about 4 months during the time before and after surgery”, Wendling shares. “After the pilot, we realized that we needed to come up with a different approach. CMS prevented us from giving the iPads to their patients, a critical population that we didn’t want to exclude. In addition, it was very expensive to have enough iPads for all patients and took a lot of work to get the iPads back.”
From the pilot, Geisinger also learned that patients wanted to use a device with everything on it. After evaluating different mobile tools, Geisinger elected to use Apple’s iBook and iTunes University to conveniently package a set of patient resources in one place and enable patients and their families to easily access and consume education content when needed, pre and post- surgery.
Geisinger began by bringing together existing components into the iBook. ”We had built a number of tools over time and were trying to leverage what we had to deliver a full ‘patient engagement package’ solution”, adds Wendling.
The Lumbar Spine patient education solution encompasses:
- Comprehensive set of interactive videos, animations, images
- MyGeisinger Patient Portal- 350k+ users with access to their patient record, visit notes and pre-visit prep
- MySurgery: Lumbar Spine reminder mobile app – Developed for the iPad loan pilot, this app reminds the patient of activities that need to be done pre and post- surgery
- Health (electronic) questionnaires for Lumbar Spine outcomes & medication reconciliation – These have been in place for a several years
Patient Education Experience & Engagement
When Geisinger patient Lisa decides to have lumbar spine surgery, she receives a handout explaining how to use her mobile device (iPhone, iPad) to access a suite of patient engagement tools through iTunes University or to download an iBook. Lisa’s friends and family can also access the educational materials to help her throughout surgery prep and recovery. The handout instructs Lisa to contact the Nurse Navigators listed with any questions.
Patient Lisa engages electronically with these educational resources which contain animations, videos and interactive components. She moves through the chapters covering “meeting the care team”, “learning about the surgery”, “diet and medication guidelines”, “what to do before surgery”, “what to expect day of and after surgery” and even ”Navigating the Geisinger Medical Center”.
Within the course, patient Lisa is encouraged to download the Lumbar Spine App to receive reminders about pre and post- surgery activities such as diet and medication requirements, what to expect during the hospital stay, things to watch for post- surgery (e.g. fever), how to address pain, exercise and sexual activity. Three and twelve months after surgery, Lisa receives a notification and logs into her patient portal to complete health questionnaires about her Lumbar Spine recovery outcomes and medication. All of the information that Lisa enters flows into the EMR so that the care team can monitor her recovery.
“We have received very positive response from our patients who like accessing these resources all in one place. It helps by setting expectations, reinforces materials discussed at clinic visits, reminds them of important steps and gives them a reference to share with family and friends. Since the 3 month visit tends to be difficult to schedule and not all providers feel it is necessary, the questionnaire responses let the team check in with the patient and follow-up if there is a need”, describes Wendling.
Geisinger has expanded this education offering beyond Lumber Spine with iBooks for Pediatric Concussion and NICU (for parents). “Pediatrics was the initial area for our IPS project (iPads while patients are in the hospital). We learned about the high-volume of print materials that are handed out in the NICU and realized that we needed to give parents a better tool”, Wendling explains.
The Geisinger in Motion & IT teams continue to tackle resource issues and have "more ideas than we can execute”. Currently, they are working through a set of operational issues for tracking and measurement:
Activity Tracking-Fitbit/Withings: Although it was part of iPad pilot (e.g. 10 patients were given a Fitbit), it is not currently in iTunes University. “We are waiting on a project where the ability to get patient generated health data from wearables will be available in the patient portal and then can automatically be uploaded into the EMR”, Wendling shares.
Measurement: “We completed and posted the Lumbar Spine course in December with an access code but then had to work with Apple to get qualified as an education institution in order to make it available publicly. From iTunes University, there have been about 30 downloads of the Lumbar Spine, 20 downloads of each of the NICU books and 16 of the Concussion. This is a public system so it is really hard to determine who is downloading. We are using survey data to better understand the profile of our users”, Wendling adds.
In the future, Geisinger plans to bring out bariatric surgery education through iBook and iTunes University. “Obesity is a significant health issue in Pennsylvania and the components around healthy weight and eating can also be used for other conditions such as diabetes, heart failure and hypertension. We hope this will be a building block as we expand our education resources to support patients and families”, concludes Wendling.
Innovative Providers Use Technology to Stay Connected with Patients Pre- Surgery through Recovery
 October 30, 2014
October 30, 2014 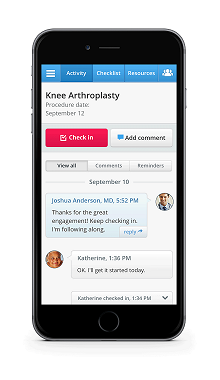 Healthloop Virtual Patient Check in
Healthloop Virtual Patient Check in
Healthcare reform has placed increased demands on doctors who are already managing increased patient loads. As a result, doctors are spending less time with their patients.
Patients are being asked to take on more responsibility in managing their care. This is particularly challenging before and after a surgical procedure. A patient typically leaves the hospital with a stack of paper discharge instructions about medications, the follow- up visit and a list of symptoms to monitor with directions to contact the doctor if problems occur. Throughout recovery, the patient is often left to figure things out because she "doesn’t want to bother the doctor". When the patient makes uninformed decisions about medications or readiness to begin an activity level, it can set her back on her recovery path or lead to costly hospital readmissions.
Other than checking in with patients during the follow- up visit, providers are in reactive mode; patients calling with complex problems or heading to the ER.
Since patient satisfaction, care quality and costs are impacted by the current process, providers are motivated to find a solution that virtually supports the patient's needs for guidance, education and shared decision making.
Virtual Patient Support
It all started in 2007 when Dr. Jordan Shlain was treating a patient who wasn’t feeling well. After discussing her symptoms, he gave the patient his cell number and asked to please call him if she felt worse by morning. He discovered a few days later that she had developed pneumonia. From this experience, Dr. Shlain learned that although he wanted to be proactive with his care, he couldn’t depend on the patient to call with an update. His began texting patients asking “do you feel the same, better or worse?” Dr. Shlain did not take any chances and assumed that a non- response from the patient indicated there may be a problem.
After speaking with providers about not really knowing how a patient is doing post discharge, they expressed interest in daily virtual interactions with the patient as a way to increase patient engagement and prevent readmissions. Patients loved the idea of interacting electronically with their doctor on a daily basis since it would give them unprecedented access to communicate concerns and address problems in a quick and convenient way. This was the backdrop that led to the development of Healthloop.
“Since late June, we have been using Healthloop for patients who have hip and knee replacement surgery”, shares Dr. Mohan, Surgeon for a large Integrated Delivery Network. “Our team was looking for a solution that would enable us to share the experience together with our patient. We also wanted to put the patient in the driver’s seat and give them control, while we were in the passenger seat as an observer and navigator.” Dr. Mohan’s orthopedic patients are on Healthloop before surgery and throughout recovery which tends to be 1-3 months.
Dr. Andrew Goldstone, ENT Surgeon at Greater Baltimore Medical Center started using Healthloop in February with his adult and pediatric patients throughout recovery which typically lasts 2-4 weeks. Healthloop electronic communications are delivered to the parents of his young patients for ongoing support. "HealthLoop, in a technologically modern way, tries to mimic the old days when we admitted patients a day or so before and kept them as many days as we or they wanted to stay after surgery. This gave patients and their families a comfort level that most current M.D.s have never witnessed. The same goes with patients who, after ambulatory surgery, pay at the next window and go home. They have no clue how patient friendly it used to be having an extended ’hand holding‘ before returning home. I view HealthLoop as an attempt to recreate that extended comfort,” explains Dr. Goldstone.
Patient Experience
HealthLoop enables the physician to support the patient before surgery and monitor him post discharge and between visits, engaging each patient “as if he is the most important person”. With the goal of delivering guidance when the patient needs it, Healthloop works closely with the provider organization to define the questions that patients ask at each step of the recovery process. Together, they review typical calls at day 1, 2, etc., determine the appropriate response and set up the schedule to deliver the information to the patient right when they need it.
Taking a closer look at the patient experience, Gary is referred by his primary care physician to a specialist about knee surgery. After deciding together to move forward with the operation, the surgeon quickly enrolls Gary in Healthloop to guide him before and after the surgery. Gary receives an email to complete his enrollment including his preferences for receiving Healthloop communications (i.e. email, text).
Before surgery, Gary answers questions about risk factors and receives guidance and checklists to prepare for his operation. For example, he learns how to to prepare his house to easily navigate when he returns home following surgery.
After surgery, Gary receives a daily electronic communication with a set of questions to understand how he is feeling (i.e. pain level, specific symptoms, problems with meds, etc.), personalized education materials, activity and medication reminders and a checklist of To Dos. Based on Gary’s feedback and progress, his care plan is updated and his next day’s check-in is automatically prepared.
Healthloop is designed for two way engagement. If Gary experiences any health problems, these are gathered through his check- in responses and trigger an SMS message to his care team for intervention and support.
With recent integration to Apple’s Healthkit, patient information is extended beyond daily check- in responses to include health tracking data. For example, Gary’s doctor has instructed him to take steps while healing from his knee operation. Gary’s tracker information is combined with his daily check-ins to give his care team more insight into his health status. Concerned about not enough movement, his clinician may call and learn that Gary is not moving enough because of his medication side effects which can be addressed through a prescription change.
Pilot Feedback; Patients & Providers
Healthloop wants to deliver a truly patient- centric communication channel and uses patient feedback to enhance the solution. After hearing a patient comment that the messages felt “too robotic” and “do not sound like they are coming from my doctor”, the communications were refined to be more conversational.
Another patient commented that the messages were using doctor’s words which resulted in changes to incorporate more patient vocabulary and experience. For example, questions about a blood clot were replaced with “feels like a cramp in my calf”.
Patient Comments
Healthloop has delivered over 57,000 daily check-ins to patients and has received positive feedback about the experience:
Guidance: “I wanted to be able to say ‘I have this” and have someone come back and say that is normal and here is the process. Then all of my negative energy goes away”, “easy way for me to make sure that I was on the track with my recovery”. “The questions promoted me to be more aware of my situation”.
Convenience: “Without Healthloop. I would have called (doctor) 5- 7 times”, “This saved me a trip to my doctor”.
Access: “It was an extension of my doctor so instead of talking to a nurse and having her get back to me, I had a direct conduit to my doctor.”
Provider Comments
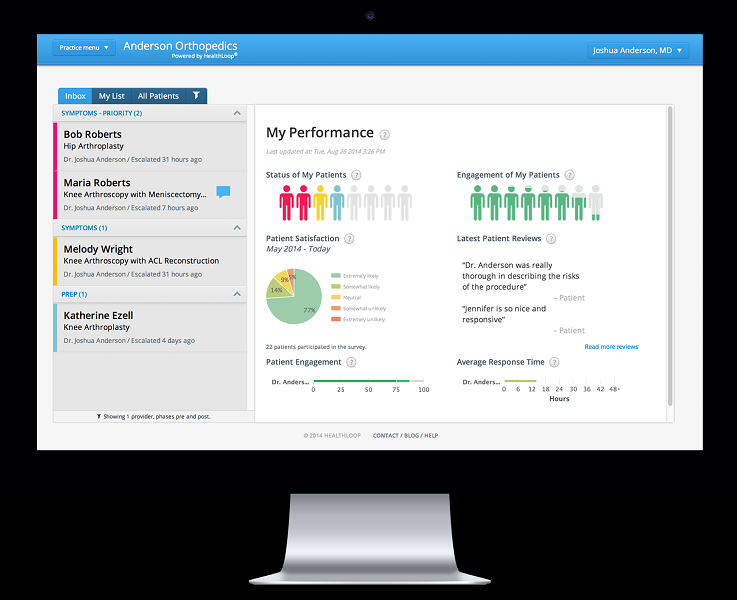 Healthloop Clinician Dashboard
Healthloop Clinician Dashboard
“As our team developed our Healthloop, we charted out what a recovery really is. With this, I know what my patient is going through, can emphasize and say with confidence that over half of my patients have their pain under control after day 4”, explains Dr. Mohan. “We also participate in a Medical Destination Program with patients traveling to our hospital, often from out of state. After staying in a hotel for 10- 14 days, they come to see me for a follow-up visit before returning home. We are now thinking about how we can use Healthloop to manage their care from a distance to make sure that the patient has a successful recovery.”
Comments from other providers:
Patient Satisfaction: “My patients told me that they looked forward to their daily Healthloop check-ins because it felt like ‘someone was watching over me’ who really cared”.
Operational Efficiency: “For my practice, the volume of calls from patients has dropped tremendously. I notice it and my staff notices it too.” “I am thinking about eliminating the 2 week follow-up visit and to just see the patient at the 6 week visit since I can check in on their pain management, incision and any other issues through Healthloop.”
Better Quality: “Helps us pick up complications much sooner. It reinforces a plan with what to do and reminders”, “We are raising the bar on care by ensuring that we are giving the patient the pre and post-surgery education and care that they need”.
Success Measures
Providers using Healthloop are evaluating a set of success factors based on their program goals. In addition to lower costs which is measured over time, providers are monitoring:
Patient Engagement; Patient Satisfaction using the net promoter score.
Better Quality; Benchmarking patient progress, measuring patient’s perceptions of care quality received
Operational Efficiency; Call reduction to the practice
Regarding patient engagement, some providers are leveraging positive ratings through social media. Patients who give the highest scores (5 Star Ratings) are encouraged to share their ratings and experiences through the link provided to public review sites such as HealthGrades and Vitals. Patients who give average or below average score are asked to explain how the provider can improve. Patients have commented on everything from old waiting room magazines to being put on hold for too long when they call.
With Healthloop, “my patients tell me that they are happy with the surgery because I was right there with them. I also notice patients are much more relaxed during their follow-up appointments. That is so important to me”, Dr. Mohan concludes.
 consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  mobile health and wellness texting,
mobile health and wellness texting,  mobile health application,
mobile health application,  online health and wellness support,
online health and wellness support,  patient ehealth engagement,
patient ehealth engagement,  self- management health tools in
self- management health tools in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  Population health management,
Population health management,  TeleHealth,
TeleHealth,  shared decision making ehealth
shared decision making ehealth Boston Children's Hospital Monitors Young Patients with Data from Caregivers; Parents, Teachers and Coaches
 September 12, 2014
September 12, 2014  Dr. Eugenia Chan sat patiently waiting for her fidgety first grade patient and her frustrated mother to answer her question. "How was the new medication working to help Janie with her ADHD"? Janie's mom hadn’t had a chance to fill out an ADHD behavior questionnaire in the chaotic waiting area, so she tried to summarize her impressions since their last doctor’s appointment a few months ago. She hadn’t heard specific feedback from Janie’s teacher, and had also forgotten to give the ADHD questionnaire to her teacher so that they would understand how she was doing in school.
Dr. Eugenia Chan sat patiently waiting for her fidgety first grade patient and her frustrated mother to answer her question. "How was the new medication working to help Janie with her ADHD"? Janie's mom hadn’t had a chance to fill out an ADHD behavior questionnaire in the chaotic waiting area, so she tried to summarize her impressions since their last doctor’s appointment a few months ago. She hadn’t heard specific feedback from Janie’s teacher, and had also forgotten to give the ADHD questionnaire to her teacher so that they would understand how she was doing in school.
In 2011, Dr. Chan, MD, MPH, a developmental-behavioral pediatrician and health services researcher in the Division of Developmental Medicine at Boston Children’s Hospital, felt that she needed a better way to monitor her patients and gather insight into how they were doing with their medications and treatment plans. With a grant from the Croll Family Foundation, Dr. Chan collaborated with Dr. Eric Fleegler, MD, MPH, a pediatric emergency medicine physician and health services researcher in the Division of Emergency Medicine at Boston Children’s Hospital, on the development of a new software tool, eDMC (electronic Developmental Medicine Center).
Their goal was to gather and interpret the information from parents and teachers more effectively and gain a more comprehensive view into patient behavior between visits. The doctor determines when the system will email the parents, typically a week or two before the appointment. When the parent receives the email with a link into the software platform, she logs in and answers a set of questions about symptoms, school performance, quality of life, global functioning and improvement since the beginning of the treatment. The parent gives the email addresses of the patient’s teachers and other important observers of the child (e.g., sports coaches, behavioral therapists, tutors) to the clinician to get them set up in the system so they can answer similar questions.
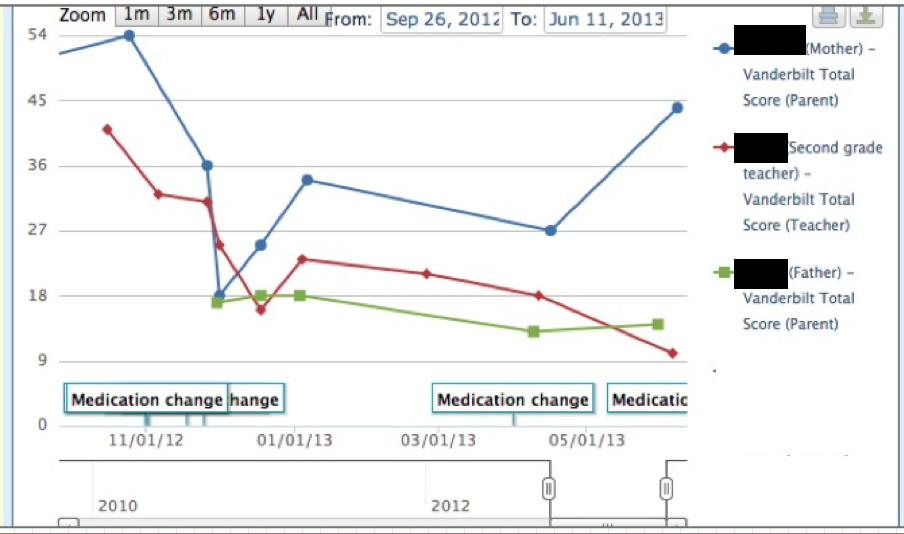 Clinicial InterfaceWith this information, Dr. Chan is able to determine how her patient is doing throughout the day, week and over time. During the visit, she shares this information with her patient and family, points out trends and discusses what has transpired. On the graphs, each line shows data from a different caregiver; parent, teacher and coach. The clinician can also drill down to see specific symptoms and their ratings that are incorporated into a score. With the treatment plan in mind, the clinician evaluates the data and focuses in on any discrepancies to determine what is really happening. This exchange supports her clinical decisions and enables her to participate in shared decision making with her patient and his family.
Clinicial InterfaceWith this information, Dr. Chan is able to determine how her patient is doing throughout the day, week and over time. During the visit, she shares this information with her patient and family, points out trends and discusses what has transpired. On the graphs, each line shows data from a different caregiver; parent, teacher and coach. The clinician can also drill down to see specific symptoms and their ratings that are incorporated into a score. With the treatment plan in mind, the clinician evaluates the data and focuses in on any discrepancies to determine what is really happening. This exchange supports her clinical decisions and enables her to participate in shared decision making with her patient and his family.
“I’ve already started using the system to work with my adolescent patients who want to go off their medications. When I agree to let them try coming off meds, I suggest that we use the questionnaires to monitor results. At the next appointment, patients are often surprised to view parent and teacher ratings and comments, that she was ‘disruptive’ or was ‘unable to pay attention’”, describes Dr. Chan.
Another feature of the platform is the ability to notify the clinician when there is a “red flag” patient problem that may require action (i.e. severe depression). Even though parents are made aware that this is not a real time monitoring system, there is someone responsible for ensuring that clinicians have seen the red flag alert.
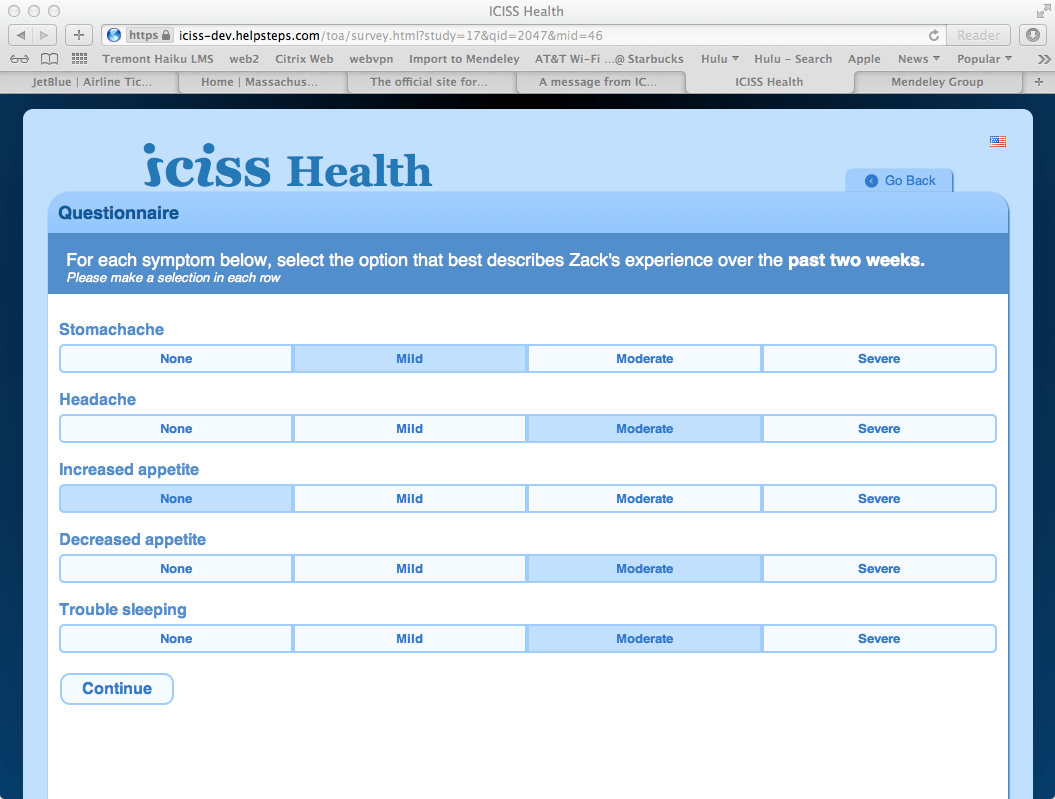 Parent InterfaceSince the program started, over 3,000 pediatric patients have participated. One parent comments on the value that she sees with the system, “it is very easy to use and I like that we save the time at the doctor’s appointment and all of the information is there”. Dr. Fleeger adds that the system “transforms how patients are interacting with their clinicians. At the appointment, the clinician can show them the graphs and tables on the computer to understand where they are and have a fruitful conversation”. Dr. Leonard Rappaport, Chief of the Division of Developmental Medicine at Boston Children’s, says that the platform “is the first major improvement we have made in individualized care for developmental disorders in the past two decades.”
Parent InterfaceSince the program started, over 3,000 pediatric patients have participated. One parent comments on the value that she sees with the system, “it is very easy to use and I like that we save the time at the doctor’s appointment and all of the information is there”. Dr. Fleeger adds that the system “transforms how patients are interacting with their clinicians. At the appointment, the clinician can show them the graphs and tables on the computer to understand where they are and have a fruitful conversation”. Dr. Leonard Rappaport, Chief of the Division of Developmental Medicine at Boston Children’s, says that the platform “is the first major improvement we have made in individualized care for developmental disorders in the past two decades.”
Currently the clinician can copy patient level summary information from the system into the EMR. Although the platform is web- based, Dr. Chan mentioned they were creating a mobile interface for access through smartphones and tablets.
Expanding ICISS Health; More Patients & Populations
In 2012, Dr. Chan and Dr. Fleeger renamed the platform the Integrated Clinical Information Sharing System (ICISS Health) to be more generalized for expansion into other pediatric patient populations.
“We have extended the ICISS Health platform to additional clinics at Boston Children’s that treat patients with ADHD, as well as private practices affiliated with Boston Children’s, and we are expanding into new conditions such as autism, asthma, depression and epilepsy”.
For each new condition, they have convened a cross disciplinary team to define the data that need to be collected to support decisions. “For example, we are working closely with clinicians from the Boston Children’s Autism Center to devise a questionnaire for patients, since there is no standardized set of questions for this patient population” explains Dr. Chan. “For asthma, we would like to invite the school nurse to participate and provide insight into frequency of nurse office visits and rescue medication use by the patient, and whether they used the patient’s asthma action plan.”
The team at Boston Children’s is in the process of collecting information to evaluate the ICISS Health platform impact on patient health outcomes and healthcare utilization and costs. Dr. Chan also mentioned their interest in calculating potential cost savings from the platform by identifying problems early and intervening in time to prevent emergency department visits and hospitalizations.
“As we think about the future of the platform, we are interested in going beyond the electronic questionnaires to capturing and integrating information from devices and mobile applications”, Dr. Chan concludes.
 Motivation for health and wellness,
Motivation for health and wellness,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  family ehealth engagement,
family ehealth engagement,  patient education,
patient education,  patient ehealth engagement,
patient ehealth engagement,  personalization for health and wellness in
personalization for health and wellness in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Consumer Segmentation Health,
Consumer Segmentation Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement
Patient Engagement Mercy Hospital Engages & Educates Patients through a Medical Destination Program
 September 2, 2014
September 2, 2014 In October 2012, Mercy Hospital Springfield of Missouri, and two other health systems launched a Centers of Excellence program with a major retailer to provide spine care for associates and their family members covered by the company’s medical plans. When an associate chooses to receive care at a Center of Excellence, they do not pay any out-of-pocket costs. In addition, the retailer picks up the tab for travel, lodging and food for the patient and caregiver. Mercy was chosen based on three factors: ethics, quality and value. Mercy Hospital is a Stage 6 Hospital in the HIMSS Analytics EMR Adoption Model (EMRAM).
The following October, Mercy Hospital Springfield added another contract with the Pacific Business Group on Health (PBGH), which includes large employers like Walmart and Lowe’s. This agreement established a Center of Excellence for knee and hip replacements.
With patients coming in from other parts of the country for various procedures, it became apparent to Mercy that patients needed some information before arriving in Springfield, Missouri. “One of the challenges that we addressed was how to effectively deliver patient education and a good patient experience when the patient is not in front of us,” explained Pam Holt, director of Patient Education and Care Management at Mercy. “We needed a way to empower remote patients with information about what will happen and what to expect during their surgery. Easing patients’ anxiety and ensuring they are comfortable is a top priority for us.”
 Mercy selected EmmiEngage, a patient engagement solution which provides an interactive health information platform certified for Stage 2 Meaningful Use for Patient-Specific Education. Each patient in the Destination Program receives an email from Mercy. The email contains a unique link enabling access via the web or mobile to customized videos with simplified medical information. Patients can view the videos many times and share them with friends and family. “Some of our older patients may go to their adult children’s homes because they don’t have a computer or they just want to watch the video together,” said Holt. “Plus, the back-end system allows our clinicians to know if patients have reviewed the educational information. If they have not, we’ll reach out to ensure the patient gets that prior education and is prepared for surgery.”
Mercy selected EmmiEngage, a patient engagement solution which provides an interactive health information platform certified for Stage 2 Meaningful Use for Patient-Specific Education. Each patient in the Destination Program receives an email from Mercy. The email contains a unique link enabling access via the web or mobile to customized videos with simplified medical information. Patients can view the videos many times and share them with friends and family. “Some of our older patients may go to their adult children’s homes because they don’t have a computer or they just want to watch the video together,” said Holt. “Plus, the back-end system allows our clinicians to know if patients have reviewed the educational information. If they have not, we’ll reach out to ensure the patient gets that prior education and is prepared for surgery.”
When traveling for care, it is particularly important for patients to prepare for discharge before hopping on the airplane. “For example, if their bedroom is upstairs, they may want to use a spare bedroom downstairs during their recovery,” Holt explains. “This information helps them think about their needs ahead of time. In fact, that’s good preparation for all of our patients, which is why we use this tool for patients who are local as well those who travel here.”
EmmiEngage provides a personalized informative overview. It is not intended to take the place of conversations between the patient and their doctor, but instead supports the relationship between them. “At Mercy, we view the solution as a technology to relay ‘general treatment’ information in an approach that suits patients’ learning style. However, we know that each patient has a unique set of circumstances that will impact their surgery and only their doctor can deliver those specific instructions,” described Holt.
Patient Related Measures
Mercy greatly values patient feedback and the responses to the program reinforces the belief that this approach is working.
“I was very impressed with the presentation! It was most helpful. Some things I already knew and it gave me some new ideas of what I can do to help myself. I have a lot more questions I will be asking my doctor the next time I see him.”
“The video was very informative and insightful. I feel I am going into this procedure with a better understanding of the procedure I am facing.”
“Rather enjoyed knowing what will happen and the risk involved. Very helpful overall”.
In addition to qualitative feedback, Mercy monitors specific patient related success measures. “We know that 85% of patients are consuming educational content through their portal. Ten percent have asked questions and 15% have contacted their doctors after reviewing the educational information. From a patient experience standpoint, 80% of patients report that the portal programs answered questions that the patient would have asked their doctor,” Holt added.
Mercy clinicians also value using technology to support patients prior to their surgery. “Patients who view a program are more prepared for their procedure and have a better understanding of their health. The benefit is two-fold: it pays off in saved clinic time and helps the patient feel more comfortable about their care,” concluded Dr. John Brown, Mercy Family and Travel Medicine.
Patient education is a key component of Meaningful Use Stage 2 but also there is growing evidence that effective patient education can impact patient outcomes as well as improve patient engagement and satisfaction. Providing these tools for patients, whether remote or local, as part of a risk sharing agreement or through traditional reimbursement, is an effective approach to patient engagement.
 Motivation for health and wellness,
Motivation for health and wellness,  care collaboration,
care collaboration,  educating consumers about health and wellness,
educating consumers about health and wellness,  family ehealth engagement,
family ehealth engagement,  online health and wellness support,
online health and wellness support,  patient education,
patient education,  patient ehealth engagement,
patient ehealth engagement,  personalization for health and wellness in
personalization for health and wellness in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  shared decision making ehealth
shared decision making ehealth Mass General Hospital Drives Patient Engagement through Multi-Specialty TeleHealth
 July 7, 2014
July 7, 2014  MGH TeleBurns TodayMassachusetts General Hospital (MGH) and parent organization Partners HealthCare have a long history in telemedicine and innovation. In 1967, Drs. Ken Bird and Jay Sanders were early pioneers in telemedicine, providing care to patients at Boston’s Logan Airport. The innovation continued in 1995 when Dr. Joe Kvedar founded the Partners Center for Connected Health (CCH). In 2001, Dr. Lee Schwamm launched the Partners TeleStroke Program, through which MGH and Brigham and Women's Hospital provide 24/7 TeleStroke care to 30+ community hospitals in New England. The program also enables other US hospitals to deliver TeleStroke services.
MGH TeleBurns TodayMassachusetts General Hospital (MGH) and parent organization Partners HealthCare have a long history in telemedicine and innovation. In 1967, Drs. Ken Bird and Jay Sanders were early pioneers in telemedicine, providing care to patients at Boston’s Logan Airport. The innovation continued in 1995 when Dr. Joe Kvedar founded the Partners Center for Connected Health (CCH). In 2001, Dr. Lee Schwamm launched the Partners TeleStroke Program, through which MGH and Brigham and Women's Hospital provide 24/7 TeleStroke care to 30+ community hospitals in New England. The program also enables other US hospitals to deliver TeleStroke services.
In 2011, MGH launched a small startup within the organization’s walls, a hospital-wide initiative called Massachusetts General Hospital TeleHealth. Building on the TeleStroke Program success and in partnership with CCH, the team is focused on achieving the goals of better, accountable, and affordable care for individual patients and populations using technology. The program enables clinicians across multiple specialties to provide high-quality, coordinated care to patients and families using familiar technology; phone, video, text, email, mobile apps and remote monitoring.
MGH has successfully embedded telehealth into patient care in several specialty areas and believes telehealth to be a mode of care delivery to help achieve the triple aim. While 21 states and the District of Columbia have laws mandating telehealth coverage under health insurance plans, Massachusetts is not among them. Given the lack of payer reimbursement, MGH is committed to paying its clinicians to provide telehealth services to patients. However, for MGH and others to expand telehealth services, universal mechanisms for funding healthcare need to align to new models of healthcare delivery.
MGH TELEHEALTH JOURNEY
“In our early days, we were willing to try most anything, and have learned a lot through trial and error and close partnership with clinicians across the institution,” says Sarah Sossong, Director of the Mass General TeleHealth program.
Building off the TeleStroke model, clinicians in Pediatrics, the Burn Center, and the Brain Tumor Program now offer emergency consults to clinicians treating patients in community hospitals. Cardiac ICU attending physicians use a robot to virtually round on patients. Multidisciplinary teams in the MGH Cancer Center conduct virtual case conferences with community hospitals. Specialists in cardiology, dermatology, and neurology provide virtual curbside consults to MGH PCPs to facilitate timely and comprehensive medical advice. “By fostering innovation in multiple areas, our goal is to identify the ‘sweet spots’ for telehealth,” Sossong explains.
The Mass General TeleHealth program continues to implement and expand virtual offerings. “Virtual visits” replace an in-person office visit using familiar technology like video and email on a smartphone, tablet, or computer. Since launching in spring 2013, 50+ clinicians across five divisions have conducted more than 1,200 video-enabled virtual visits with existing MGH patients in their homes and other settings.
TelePsychiatry
 MGH TelePsychiatryMass General’s Department of Psychiatry was one of the first to launch video-enabled virtual visits to patients in the home, with a focus on children and adolescents with autism spectrum disorder under the clinical leadership of Dr. Janet Wozniak , associate director of the Bressler Program for Autism Spectrum Disorders at MGH and director of the Child and Adolescent Outpatient Psychiatry service. Dr. Wozniak calls virtual visits an “outstanding addition” to her clinical practice. Following autism pilot success, virtual visits rolled out with patients across 20+ disease conditions including depression, anxiety, and ADHD. “One surprising finding has been that patients who spoke very little during office visits have become more open and able to discuss their symptoms via video,” explains Wozniak.
MGH TelePsychiatryMass General’s Department of Psychiatry was one of the first to launch video-enabled virtual visits to patients in the home, with a focus on children and adolescents with autism spectrum disorder under the clinical leadership of Dr. Janet Wozniak , associate director of the Bressler Program for Autism Spectrum Disorders at MGH and director of the Child and Adolescent Outpatient Psychiatry service. Dr. Wozniak calls virtual visits an “outstanding addition” to her clinical practice. Following autism pilot success, virtual visits rolled out with patients across 20+ disease conditions including depression, anxiety, and ADHD. “One surprising finding has been that patients who spoke very little during office visits have become more open and able to discuss their symptoms via video,” explains Wozniak.
TeleNeurology
 MGH TeleNeurologyMass General’s Department of Neurology has been an early adopter of virtual visits for patients with benign conditions like migraines, and others for which long-distance travel can be challenging (i.e. Lou Gehrig's disease, stroke, multiple sclerosis, muscle diseases, movement disorders, seizures).
MGH TeleNeurologyMass General’s Department of Neurology has been an early adopter of virtual visits for patients with benign conditions like migraines, and others for which long-distance travel can be challenging (i.e. Lou Gehrig's disease, stroke, multiple sclerosis, muscle diseases, movement disorders, seizures).
Dr. Adam Cohen, TeleNeurology and Neurology’s inpatient director, comments that “virtual visits allow us to see our patients from every corner of the state. The ease of virtual visits offers huge benefits to our patients who no longer have to trek into Boston and also for our patients who have difficulty traveling. Virtual visits also make it easier to check-in with our patients, often for just a few minutes.”
TeleCardiology
 MGH TeleCardiologyDr. Stephanie Moore in Mass General’s Heart Center has been pioneer of telehealth through her work in remote monitoring for Heart Failure patients with CCH. Remote monitoring has become standard practice for many heart failure patients discharged home. Dr. Moore has incorporated virtual visits into patient care to facilitate patient education by her nursing team and is exploring how virtual visits can work with other virtual tools like remote monitoring.
MGH TeleCardiologyDr. Stephanie Moore in Mass General’s Heart Center has been pioneer of telehealth through her work in remote monitoring for Heart Failure patients with CCH. Remote monitoring has become standard practice for many heart failure patients discharged home. Dr. Moore has incorporated virtual visits into patient care to facilitate patient education by her nursing team and is exploring how virtual visits can work with other virtual tools like remote monitoring.
Dr. Ami Bhatt, a specialist in treating adult congenital heart disease, has found virtual visits enhance patient care. “My patients are busy and often live several hours away. A quick visit to review test results ends up being costly, and a call is not enough to explain results and educate patients to be their own advocates.” With virtual visits, Dr. Bhatt walks patients through their heart images and test results.
TeleBurns
At the MGH Burn Center, Dr. Shawn Fagan developed a successful program providing follow-up care to patients at Boston’s Spaulding Rehabilitation Hospital. The program has benefited many patients including Boston Marathon bombing survivors treated at MGH and subsequently treated at Spaulding. With Spaulding’s telemedicine nurse, the patient connects to the TeleBurns team with a virtual visit instead of a trip to MGH.
One patient shared that “staying in contact with Dr. Fagan from the convenience of Spaulding was huge. It was like talking to him face-to-face. He had the equipment to see me, make decisions and treat me.”
MGH TELEHEALTH SUCCESS EVALUTATION
Healthcare providers at MGH and elsewhere have shown that telehealth lowers costs when compared with traditional in-office visits. There is also a significant improvement in patient access to medical expertise, convenience, and care quality through collaborative care opportunities that otherwise would not exist in specific clinical case scenarios.
In the first few years, the MGH TeleHealth team worked on building and implementing scalable technology platforms and integration with existing clinical workflows. “The past year has been focused on feasibility and adoption by patients and clinicians, and feedback from both groups has been overwhelmingly positive. As we continue to expand the program, long-term sustainability is our top priority,” says Sossong.
Patient Experience & Satisfaction:
 Overall, patient feedback about the telehealth experience has been very positive. The clinical team has learned that virtual visits are most successful with patients who have frequent touch points with the healthcare system or who are geographically distant.
Overall, patient feedback about the telehealth experience has been very positive. The clinical team has learned that virtual visits are most successful with patients who have frequent touch points with the healthcare system or who are geographically distant.
“The virtual visits have helped me save on gas, parking, and still achieve what we want to achieve”, shares one telehealth patient. With virtual visits, “I have my doctor in my living room, and I feel like we're a team.”
“Our early surveys show high rates of satisfaction and willingness to pay,” Sossong adds. “While there aren’t any national benchmarks for patient satisfaction with telehealth, we have patient feedback on virtual visits around quality, privacy, ease of use of the technology, and satisfaction (i.e. CAHPS). While it’s not an apples-to-apples comparison, initial patient feedback about the virtual visit experience in selected domains reflects higher satisfaction rates than in-person visits.”
Clinician and Department Experience:
Clinicians across multiple programs have also found that virtual visits allow them to stay focused on delivering patient -centered care.
Specialists providing follow-up care for patients discharged to Boston’s Spaulding Rehabilitation Hospital typically take the shuttle between MGH in Boston and Spaulding. By enabling MGH specialists to conduct virtual visits with patients at Spaulding, patients receive more timely clinical care, and specialists have additional time to see patients in clinic, instead of sitting on a shuttle.
One high-volume medical practice reported that patients receiving care through virtual visits were more likely to show up for their scheduled appointments, reducing the overall no-show rate for the department. The practice manager explains, “Like anything, it takes time to learn a new way of doing things, but we’re excited to see how virtual visits become incorporated into standard medical care as clinicians and patients become increasingly comfortable with the technology and processes”.
FUTURE TELEHEALTH DIRECTION
The MGH TeleHealth team is developing plans to expand the program in 2015. “In the coming year, our goal for video-enabled virtual visits is to more fully integrate them into the standard practice of care by deepening adoption in existing departments and expanding to new departments. In the future, there are a number of exciting possibilities,” says Sossong.
Multiple Modalities: “While there is tremendous value in interventions using a single technology, such as video-enabled virtual visits, I’m eager to explore how we can design a seamless, convenient, patient-friendly experience by putting all the pieces together. For example, a patient being treated by a psychiatrist for depression could have a treatment plan which includes using an app for tracking mood changes throughout the day, receiving text reminders about medication or an upcoming appointment, exchanging emails with the clinician about symptoms in between visits and conducting a video-enabled virtual visit for therapy, or checking in on medication symptoms. When it’s necessary to be ‘touched’ by the healthcare team, the patient can come into the office for an in-person office visit.”
Patient Education: “While our current work is focused on everything that goes into making the video-enabled virtual visit happen, there’s interest in exploring related educational tools for patients as well. For example, a recording of the virtual visit, or even the in-person visit, could be helpful as an educational tool for patients and families to review once settled back home. I can envision a future where we’ll discharge surgery patients with online portal access to a recording of their own clinician’s instructions for post-operative care, which could be one of a suite of tailored educational tools including condition specific videos or articles, or even seasonal tools for things like cold/flu season.”
The MGH TeleHealth team is determined to identify where telehealth can work to bring care access, convenience, and education to patients. “People bank online, shop online and Skype with family and friends online. Patients will start to expect to receive healthcare this way too,” Sossong concludes.
 care collaboration,
care collaboration,  educating consumers about health and wellness,
educating consumers about health and wellness,  online health and wellness support,
online health and wellness support,  patient education,
patient education,  patient ehealth engagement in
patient ehealth engagement in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Portal,
Patient Portal,  Personalization eHealth,
Personalization eHealth,  TeleHealth,
TeleHealth,  shared decision making ehealth
shared decision making ehealth