Entries in personalization for health and wellness (23)
UnitedHealthcare Empowers Caregivers with Personalized Tools for Guidance, eCommerce & Connection
 February 26, 2016
February 26, 2016 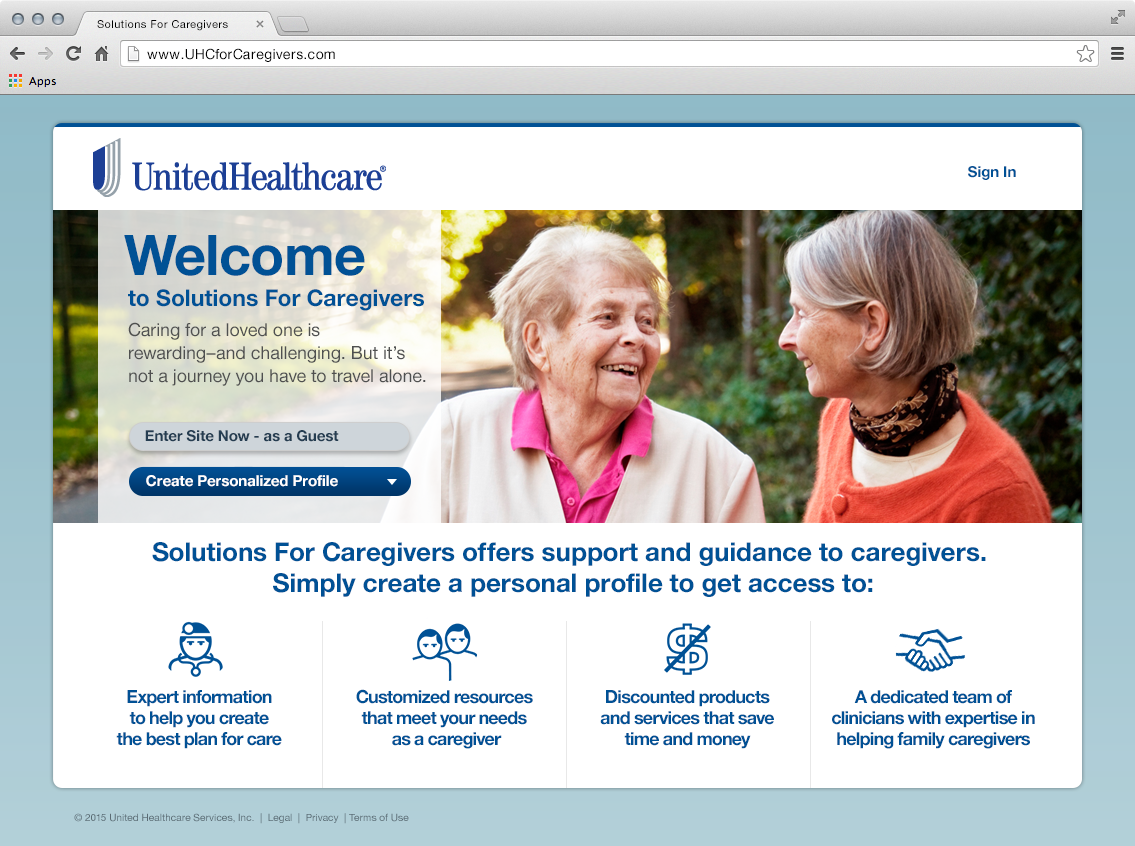 At the 2016 Consumer Electronics Show (CES) in January, UnitedHealthcare launched Solutions for Caregivers, an online program that provides resources for caregivers and their family; personalized information, a discounted marketplace of products and services and care circle community for ongoing support.
At the 2016 Consumer Electronics Show (CES) in January, UnitedHealthcare launched Solutions for Caregivers, an online program that provides resources for caregivers and their family; personalized information, a discounted marketplace of products and services and care circle community for ongoing support.
UnitedHealthcare is addressing the evolving needs of a large population of caregivers. According to the Caregiving in the U.S. 2015 report by the National Alliance for Caregiving (NAC) and AARP Public Policy Institute, an estimated 43.5 million adults have provided unpaid care during the prior 12 months, 34.2 million (79%) offering care for an adult age 50+.
“Many caregivers are searching for relevant resources but often don’t know where to start. Solutions for Caregivers addresses the needs of family caregivers through case management services and online resources that help caregivers more effectively care for their loved ones,” shares Dr. Richard Migliori, EVP and Chief Medical Officer, UnitedHealth Group.
Caregiving Burden
According to the Caregiving in the U.S. 2015 report, caregivers spend an average of 24 hours each week helping their loved ones. Many caregivers experience their own physical, emotional and financial strain as a result of their caregiving role. Half of the caregivers indicated “they had no choice in taking on their caregiving responsibilities,” and 40% report being in high-burden situations. When asked about their health, 17% said ”it is fair or poor”, compared with 10% of the general adult population.
Many caregivers (60%) admit they had to make a workplace accommodation, such as taking time off or reducing work hours. On average, caregivers assist with “4.2 out of 7 Instrumental Activities of Daily Living (IADLs),” including transportation, grocery/other shopping, or housework. Most caregivers (84%) report an interest in receiving more information such as “keeping their loved one safe at home” and “managing their own stress.”
UnitedHealthcare has conducted extensive research with family caregivers to understand their challenges around caring for a loved one. Vidya Raman-Tangella, M.D., head of UnitedHealthcare’s Innovation Center of Excellence, explains, “We heard that each journey is a ‘unique’ and ‘personal’ experience. Family caregivers are often not prepared and do not know where to begin, which causes anxiety. Some caregivers need support recognizing ‘what is good’ when making decisions for their loved one. Finally, UnitedHealthcare heard that the family caregivers did not want to feel alone and wanted to work together with others in their care circle.”
 CAREGIVERS MARKETPLACEVidya and her innovation team set out to define a solution based on these caregiver needs. The team started with a portal front end to house a set of tools to help caregivers:
CAREGIVERS MARKETPLACEVidya and her innovation team set out to define a solution based on these caregiver needs. The team started with a portal front end to house a set of tools to help caregivers:
Personalized Information – educational articles and videos that are tailored to the specific medical issues and needs of the care recipient and caregiver. UnitedHealthcare’s articles support the topics requested by caregivers (i.e. safety, stress). Users can save an article for future reference or share with others (i.e. siblings, health coach and clinician).
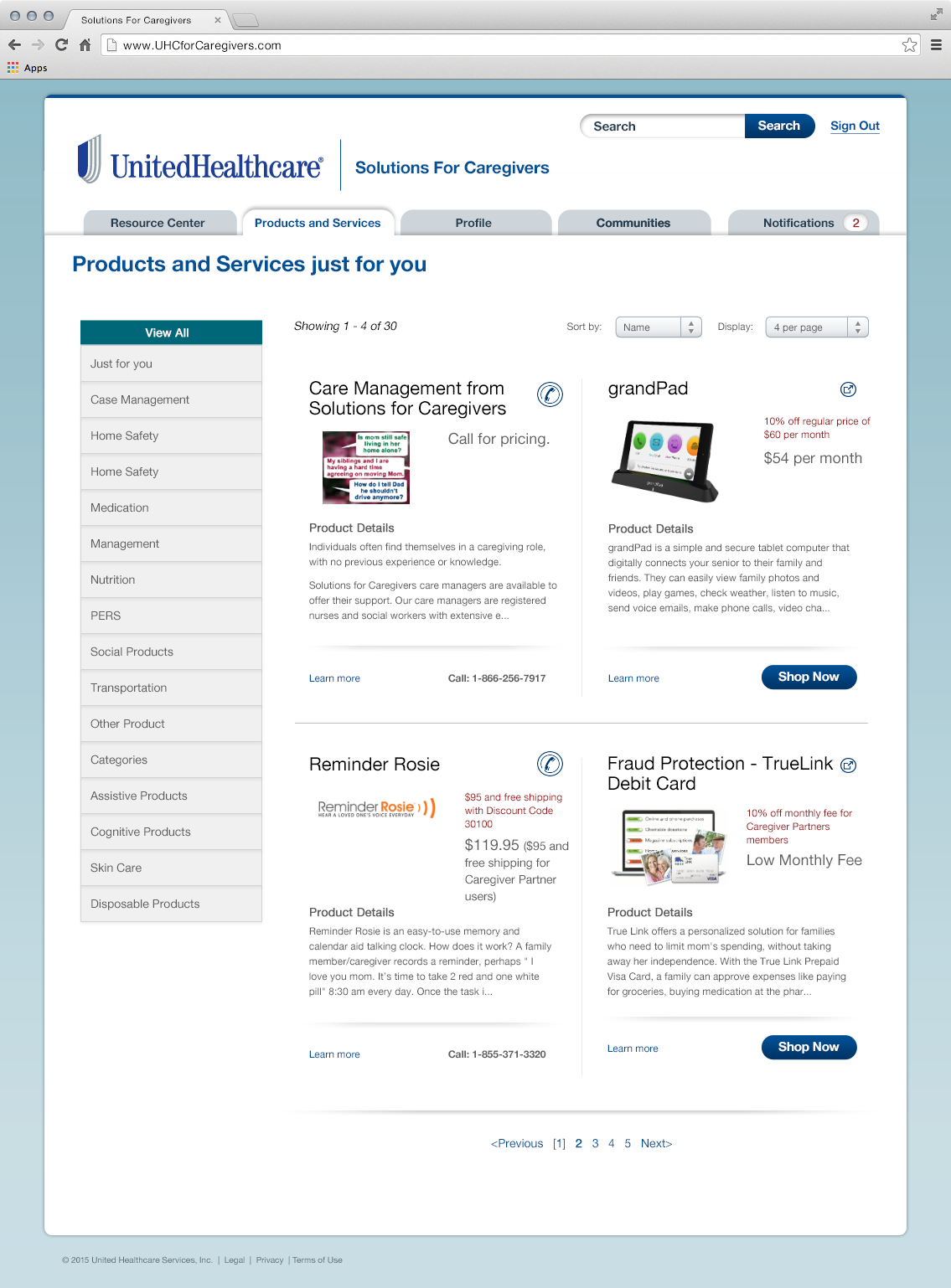
Marketplace – set of vetted discounted products and services to support the caregiver and care recipient’s conditions and challenges. Product categories include “assistive products”, “home monitoring”, “home safety” and “medication management.” Service categories span “financial”, “in-home care”, “nutrition” and “transportation”. Regarding “nutrition,” caregivers can order meals that are tailored to the care recipient’s health condition (i.e. low salt, low sugar). UnitedHealthcare’s marketplace is designed to support caregivers for activities they undertake on a regular basis, including transportation, shopping and house work.
One service option is for a “Care Manager” who can help the family plan or respond to care recipient/caregiver needs, via online, phone or consult (secure messaging). Some caregivers may have a health plan benefit that covers the care manager service, while others have the option of paying the hourly fee.
Currently, UnitedHealthcare has mostly national companies and a growing number of regional and local offerings in the marketplace. Based on the care recipient’s zip code, there may be a national service provider such as CareLinx, which offers services in the specified geography.
Community Support – centralized place where caregivers and friends of a loved one can connect, share insights and concerns (i.e. how does mom look today), add and view medical appointments & meetings on a daily/weekly/monthly calendar, post and assign tasks (i.e. a ride to the doctor’s appointment) and access a library of documents such as medication lists, doctors list, health records and a living will. The solution serves as a repository of this information, however there is no integration with the EMR or any clinical information
Caregivers can also invite others, such as clinicians and in-home caregivers, and enable them to securely access information and communicate on a common platform.
Although other companies promote online caregiver offerings today, UnitedHealthcare has designed a 'personalized caregiver solution'. During the sign-up process, the caregiver creates a profile by responding to set of questions about the care recipient; relationship, age, zip code, conditions and challenges. The caregiver also indicates their own health conditions and challenges.
For example, when family caregiver Carla responds that her 86-year-old mother has hypertension and diabetes and is dealing with mobility issues, and she (the caregiver) is experiencing depression, Carla will see articles, videos, products and services that are relevant to both of their needs.
Caregiver Solution Pilot
UnitedHealthcare is providing the Solutions for Caregivers program to large employers at no additional cost for employees to access the online services. As of January 2016, Solutions for Caregivers is being promoted to over 1 million employees. Currently, Solutions for Caregivers is also accessible to the public. For people using the employer-sponsored version, the company can cover the costs associated with care management services, enabling caregivers to access more holistic support. In comparison, people accessing the consumer site, or instances where the employer has not purchased the additional care management services, can pay out of pocket for these resources. In both versions, caregivers can access customized content, shop from the marketplace, and use the myCommunity resources.
UnitedHealthcare has received positive comments about their Caregiver solution, that it “saves time” and they would “recommend it to other caregivers”. To date, UnitedHealthcare has also noticed that many users are in the early stages of caregiving.
Future Solutions for Caregivers
“While it will take the rest of 2016 to build the volume of users, we will continue to grow our marketplace through strategic partnerships with product and service companies. We are especially interested in technology solutions for caregivers”, shares Dr. Vidya Raman-Tangella.
UnitedHealthcare is planning to leverage all customer service touch points to identify caregivers who are currently moving along the care journey or will be on the journey soon as potential users of the solution.
“Throughout the year, we will learn how this program is delivering value to caregivers and care recipients. With Boomers turning 70, we will be particularly interested to see how our offering will be used to support the boomers as they retire as well care for their loved ones”, explains Dr. Raman-Tangella.
“This program and others from UnitedHealthcare are making it easier and more convenient to people to take charge of their health and the health of their loved ones. By using technology and personalized resources, we are helping people to live healthier lives”, Dr. Migliori concludes.
Ochsner Leverages Retail, Connected Health Tools & Apple Watch to Engage Consumers
 July 6, 2015
July 6, 2015 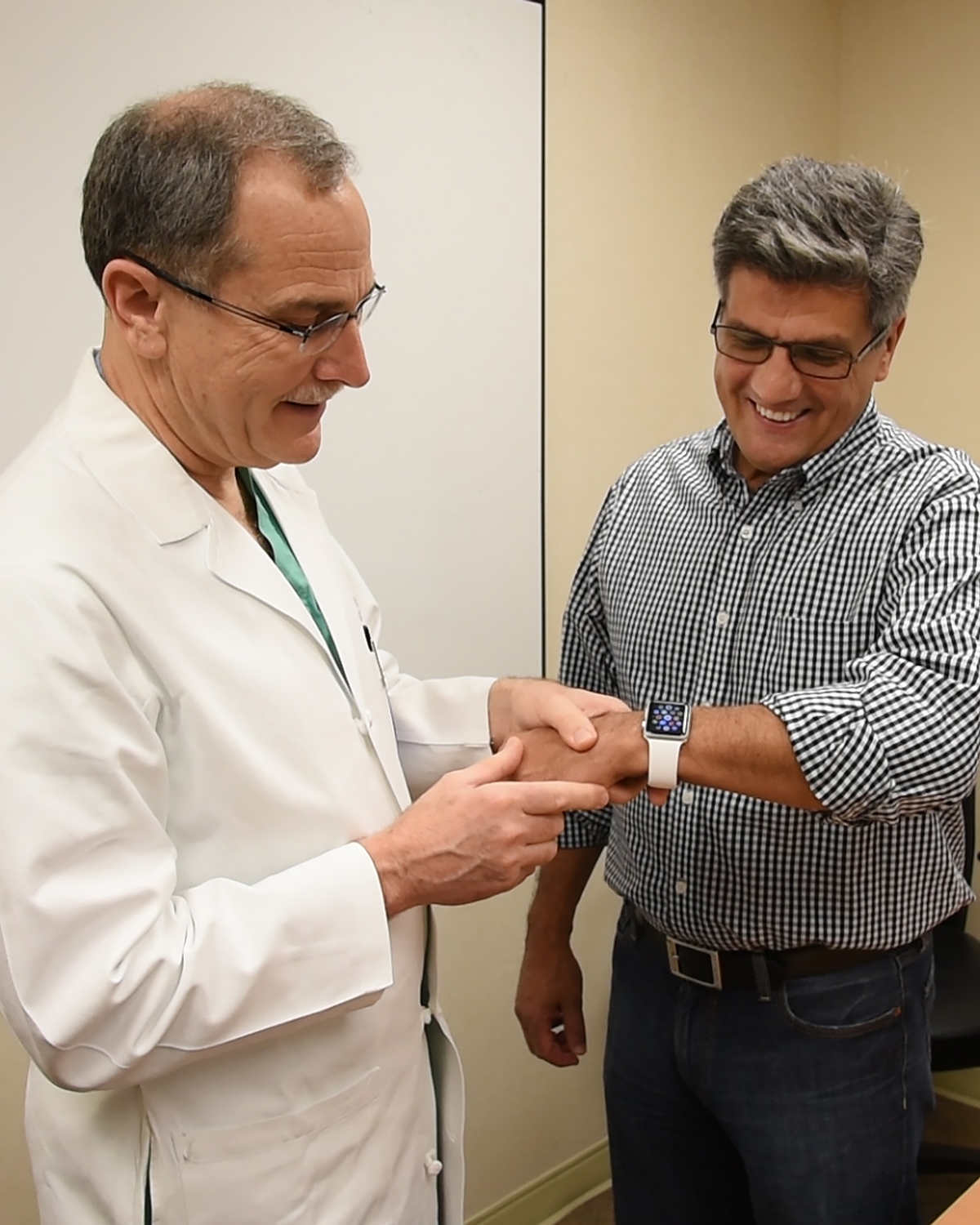 Dr. Milani with longtime patient Andres Rubiano, pilots Apple WatchDuring the last eighteen months, the Ochsner Health System has moved into new territory, meeting consumers where they are, from their OBar, a retail genius format to patient hypertension pilots with the Apple Watch to drive behavior change.
Dr. Milani with longtime patient Andres Rubiano, pilots Apple WatchDuring the last eighteen months, the Ochsner Health System has moved into new territory, meeting consumers where they are, from their OBar, a retail genius format to patient hypertension pilots with the Apple Watch to drive behavior change.
As an innovative healthcare organization, Ochsner, a large Louisiana- based health network with 12 hospitals, 40 clinicians and an a 1,000+ Physician Group Practice, is committed to helping consumers use mobile and wearable connected health tools for self- management and care collaboration
It all started back in late 2013 when Dr. Richard Milani, now Chief Clinical Transformation Officer and Vice Chair of Cardiology at Ochsner, observed what was going on nationally, a tremendous growth of mobile phone and smart apps. “At the time, I noticed that a lot of people didn’t know much about the health apps and wearables or were fearful about how to use them. My background is in preventive medicine”, explains Dr. Milani. “I saw a powerful opportunity for Ochsner to empower consumers to use mobile technology to enhance their health, opening the door to favorable behavior change.”
OBar, Retail Genuis Bar with Apps & Devices
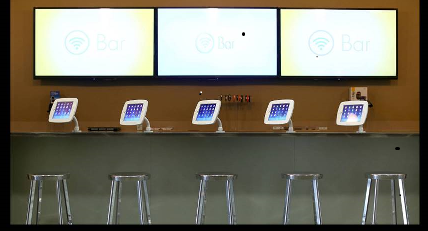 After more than nine months of planning, Ochsner launched their OBar in early 2014 at the new Ochsner Center for Primary Care and Wellness. The OBar is located in the lobby to attract people walking by as well as patients. The retail store is welcoming with digital tablets loaded with vetted mobile apps to support consumer health, “non-clinical” genius types to answer questions, provide guidance and sell discounted devices (i.e. Activity Tracker, wireless scale, blood pressure cuff and glucometer). “We created this retail setting to show people how to make themselves healthier on their own, independent of their health system. We also felt that as a health system, we could show you which health apps were good and can help you get the app loaded on your phone to begin using it.”
After more than nine months of planning, Ochsner launched their OBar in early 2014 at the new Ochsner Center for Primary Care and Wellness. The OBar is located in the lobby to attract people walking by as well as patients. The retail store is welcoming with digital tablets loaded with vetted mobile apps to support consumer health, “non-clinical” genius types to answer questions, provide guidance and sell discounted devices (i.e. Activity Tracker, wireless scale, blood pressure cuff and glucometer). “We created this retail setting to show people how to make themselves healthier on their own, independent of their health system. We also felt that as a health system, we could show you which health apps were good and can help you get the app loaded on your phone to begin using it.”
 Doctor gives patient RX for App, directs to OBar Ochsner wanted to go further, tying the OBar into their primary care services. Dr. Milani and his team created a prescription pad for their PCP offices, which lists the types of available apps and devices. The doctor simply checks off, hands the patient a prescription pad sheet and directs him downstairs to the OBar. Since this extension into primary care, clinicians have heard back from their patients about how the apps and devices have helped them make better health choices around activity, diet and their disease. Patient feedback has motivated these clinicians to tell others about the OBar.
Doctor gives patient RX for App, directs to OBar Ochsner wanted to go further, tying the OBar into their primary care services. Dr. Milani and his team created a prescription pad for their PCP offices, which lists the types of available apps and devices. The doctor simply checks off, hands the patient a prescription pad sheet and directs him downstairs to the OBar. Since this extension into primary care, clinicians have heard back from their patients about how the apps and devices have helped them make better health choices around activity, diet and their disease. Patient feedback has motivated these clinicians to tell others about the OBar.
Dr. Milani went on to explain that the OBar initiative is not designed to be a profit center. As a non-profit, Ochsner is most interested in helping people stay healthy and has invested in a retail format as a way to be sticky to attract and keep consumers coming back. As with any retail store, visitors walk in and out which makes it challenging to capture and measure the value that consumers have gained from using these apps and devices. Through anecdotes, however, Ochsner has heard about the weight loss, the knowledge about “buying the right foods” and the ability to better “understand my disease”, which has helped many consumers visiting the OBar.
Apple HealthKit & Epic Integration for Connected Health
Ochsner was the first hospital to integrate the Apple HealthKit with their Epic system. This integration powers their Connected Health programs. While the patient is still in the hospital, she is given a tablet to answer a detailed questionnaire. Hypertensive patients, for example, are asked sodium consumption, medication adherence and affordability, social situations, depression, physical activity, BMI, sleep, Health literacy, Patient activation and more. Ochsner believes that patients respond more truthfully to the tablet.
“We are phenotyping patients based on their specific disease and psycho- social measures that are fed into algorithms to personalize the care plan and decision support tools”, Dr. Milani explains. “Ochsner started with Heart Failure in early 2014, with a program for CHF patients to avoid readmissions through weight monitoring. In February 2015, we launched our Hypertension Digital Medicine Program, monitoring blood pressure and heart rate. “With the HealthKit/Epic integration, we are able to use the patient’s unique responses to the survey combined with the monitoring data to tailor the intervention to the individual”, adds Dr. Milani. Ochsner care providers monitor the dashboard to determine which patients are the priority today and to see the task check list for action.
The national data reflects that currently, only 50% of individuals diagnosed with hypertension (high blood pressure) have their blood pressure under control, or at goal. Lack of achieving goal blood pressure means that these individuals have significantly higher rates of stroke, heart disease and kidney failure. Ochsner has enrolled only patients that have failed to meet control blood pressure goals, and using this integrative approach, has achieved more than 60% control rates within 2 months.
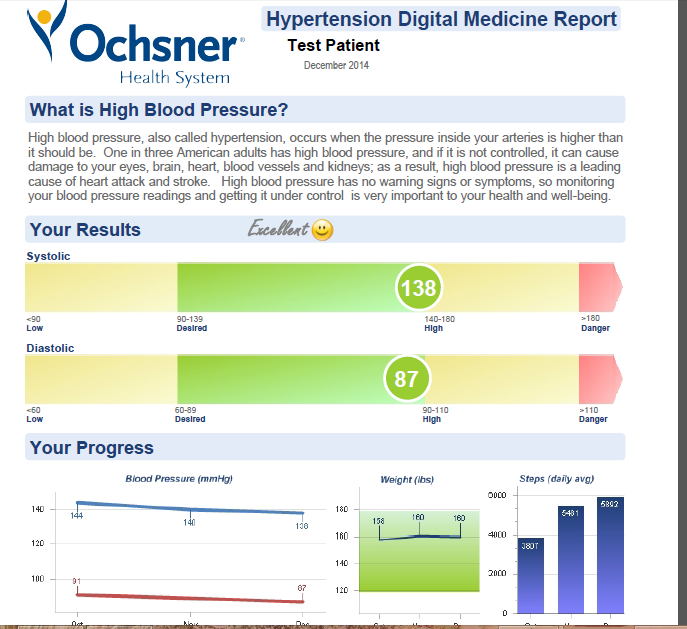 Dr. Milani and his team wanted the patient to see his progress in the program and designed an insightful report, which visually displays results and progress, quantifies risk and describes how the patient can reduce that risk. This program report is available in the patient portal and is also mailed monthly to the patient. “We decided to mail the report because we wanted the patient to have the opportunity to share the report with their family and to have the discussion about how they are doing in controlling their blood pressure in order to strengthen every day support”, admits Dr. Milani.
Dr. Milani and his team wanted the patient to see his progress in the program and designed an insightful report, which visually displays results and progress, quantifies risk and describes how the patient can reduce that risk. This program report is available in the patient portal and is also mailed monthly to the patient. “We decided to mail the report because we wanted the patient to have the opportunity to share the report with their family and to have the discussion about how they are doing in controlling their blood pressure in order to strengthen every day support”, admits Dr. Milani.
In addition to the program report, program participants receive ongoing mobile texts for motivation and encouragement.
Ochsner closely tracks, monitors and has presented very positive patient outcomes of their Integrated & Connected Health programs. One interesting insight that Dr. Milani has shared is that these participants are more successful in the beginning when they have the OBar support. “A Hypertensive patient can go to our OBar, get the program app downloaded on her phone and a demonstration about how to use the devices. This is especially important with older patients who may not feel comfortable getting set up over the phone. We realize the importance of providing this face to face technology support for our Connected Health program and are adding OBars to our other regions”, confirms Dr. Milani. Ochsner is planning to launch three more retail OBars by the end of the year.
Apple Watch for Patient Pilot
Dr. Milani views the Apple Watch as a behavioral change tool. As a foundation, this is a wearable, with many non-health features which captures the consumer’s attention and motivates consumer engagement. It takes the consumer’s focus off the phone and onto the wrist to communicate time as well as personal and professional messages.
Ochsner is designing a study to understand the potential for changing the consumer’s behavior around health. They will be enrolling hundreds of hypertensive patients with the goal of increasing physician activity and improving medication adherence.
Dr. Milani mentioned two of the health related Apple Watch apps which he plans to incorporate to help patients achieve the pilot goals. “There is a WebMD app which is a great medication reminder. It taps you on your wrist and shows you the picture of the pill that you need to take at that time. This is important because 50% of patients with chronic disease do not take their medications as prescribed. The second built-in app is for physical activity which can be used to set goals. It will tap me and remind me to stand up every 50 minutes. I can also see how I am doing against my activity goals”, shares Dr. Milani.
For the Apple Watch pilot, Ochsner will compare the outcomes and behavior change for patients in their Hypertension Digital Medicine Program with a subset of patients who also have the Apple Watch medication and activity reminders and tracking. Throughout the pilot, Dr. Milani and his team will be closely monitoring whether and how these apps impact positive patient behavior change.
 consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  health coaching,
health coaching,  mobile health and wellness texting,
mobile health and wellness texting,  personalization for health and wellness,
personalization for health and wellness,  wearables health in
wearables health in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  Population health management,
Population health management,  Retail Health Strategies,
Retail Health Strategies,  TeleHealth
TeleHealth Carolinas HealthCare’s Diabetes Patients Collaborate with Coaches Using Data from Smartphones and Devices
 April 13, 2015
April 13, 2015 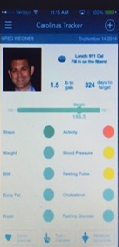 Carolinas Healthcare System, the second largest public, not-for-profit healthcare system in the U.S. (39 hospitals, 900 care locations) based in the Southeast, is committed to using technology to engage patients for better care. Last Fall, Carolinas HealthCare launched their Virtual Visit initiative to bring convenience to patients. Like other innovative healthcare systems, Carolinas HealthCare also launched a mobile app for patients to access their portal (MyCarolinas), inform about the closest urgent care location with wait times as well as offer a provider search.
Carolinas Healthcare System, the second largest public, not-for-profit healthcare system in the U.S. (39 hospitals, 900 care locations) based in the Southeast, is committed to using technology to engage patients for better care. Last Fall, Carolinas HealthCare launched their Virtual Visit initiative to bring convenience to patients. Like other innovative healthcare systems, Carolinas HealthCare also launched a mobile app for patients to access their portal (MyCarolinas), inform about the closest urgent care location with wait times as well as offer a provider search.
“This was just the beginning,” explains Pamela Landis, AVP Information Services at Carolinas HealthCare System. “We wanted to go beyond supporting patients when they needed care to becoming part of our patients’ every day health.”
Based on the market trends showing consumer’s increasing use of both mobile and social media, Carolinas HealthCare System decided to invest in technology to provide ongoing information and support. While conducting marketing research, Carolinas HealthCare learned about consumers use of different wearables and tools to track activity, fitness, nutrition, sleep and health issues and heard about their frustrations having information housed into various apps. For instance, a person could be tracking their activity in Runkeeper and using a Bluetooth-enabled scale and blood pressure cuff. All that data is being stored in separate apps.
“We wanted to address their needs, giving them a holistic view of their health by bringing together information from all of their trackers. We leverage the health kits from the major smartphone platforms for the information aggregation,” shares Landis.
“The first app, Carolinas Tracker, available in both the Apple and Android stores, enables consumers in the community to aggregate their health data from apps and devices into one place and view a dashboard to see where they need to focus their attention (i.e. be more active and manage their health conditions).” Carolinas Tracker gives people an easy way to track their health and provides clinical context around how they are doing. Consumers can not only see how many steps they have done through their Fitbit data but also whether that is enough to reach their goals through their Carolinas Tracker dashboard.
The second app, MyCarolinas Tracker for Carolinas patients, will enable patients to bring together the same tracking information as the consumer app but will also integrate with their lab data in their patient portal. This patient app will also have goal setting capabilities and enable some patients to collaborate with their health coaches.
New Tool for Diabetes Patient & Coach Care Collaboration
Carolinas HealthCare System is planning a program to provide this new mobile app to diabetes patients, given the size of the diabetes patient population at Carolinas (90k patients), significant rise in Type 2 diabetics, the impact on other diseases and long term impact on a patient’s health.
“We are envisioning an ongoing program (i.e. not a pilot) and want to learn from the early adopters. We plan to invite patients through their physician practice and through our coaching program,” Landis adds.
Success Measures for Diabetes Coaching App Program
After launching the Diabetes program, Carolinas HealthCare System will look at “adoption metrics” since this type of technology is still in the early stage of use in the market. With many health apps today downloaded and not used, Carolinas HealthCare is interested in seeing app usage such as when and how the app is being used.
“We want to see if patients will integrate the app into their life to live better by taking ownership of their health,” explains Landis.
Carolinas HealthCare is planning to collect qualitative feedback from consumers and patients through surveys and focus groups to see if/how the app has helped the patient better understand their health and whether it has made the patient feel more in charge of their health.
“We are very interested to hear about the patient’s motivation to use the app and understand triggers, actions and rewards. We want to explore social influence. For example, do the social capabilities with family/friends/care circle help the patient stay more engaged and does this make her more motivated to use the app? Carolinas Healthcare will also look at hard core usage stats – usage/how often,” Landis explains.
"When thoughtfully designed and deployed, technology can enhance the relationship of patients with their health and their healthcare team. The solutions we are building will promote empowered patients and collaborative care delivery," explains Dr. Gregory Weidner, an internist at Carolinas Healthcare System in Charlotte, N.C. . Dr. Weidner is also the medical director for Primary Care Innovation and Proactive Health and brings vision and leadership to ambulatory care redesign and digital patient engagement initiatives.
 Motivation for health and wellness,
Motivation for health and wellness,  chronic care management,
chronic care management,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  patient generated health data,
patient generated health data,  personalization for health and wellness in
personalization for health and wellness in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Portal
Patient Portal Novant Health Deploys Mobile App to Monitor Behavioral Health Patients and Proactively Provide Support
 October 9, 2014
October 9, 2014 
According to The Agency of Healthcare Research and Quality (AHRQ), an estimated “44 million people 18 and over suffer from mental disorders.” Further, “major depressive disorder is the leading cause of disability among adults”. This is a major concern for healthcare providers throughout the United States. As more patients struggle to manage their mental health condition, they are showing up in emergency rooms, where they are finding staff and systems ill equipped to deliver the specialized care that they so desperately need. This missed opportunity not only creates a negative experience for patients but also drives up healthcare expenses for providers.
Novant Health, one of the largest healthcare systems in the country (15 hospitals, 350+ physician practices in NC, SC, VA, & GA), is proactively helping behavioral health patients, reducing readmissions and preventing costly emergency room visits.
In 2013, Novant Health partnered with behavioral analytics company Ginger.io on a successful depression program in a Novant perinatal clinic. In 2014, Novant Health expanded the partnership with Ginger.io to address the unique needs of adult patients with depression by developing a customized care solution for this historically underserved population.
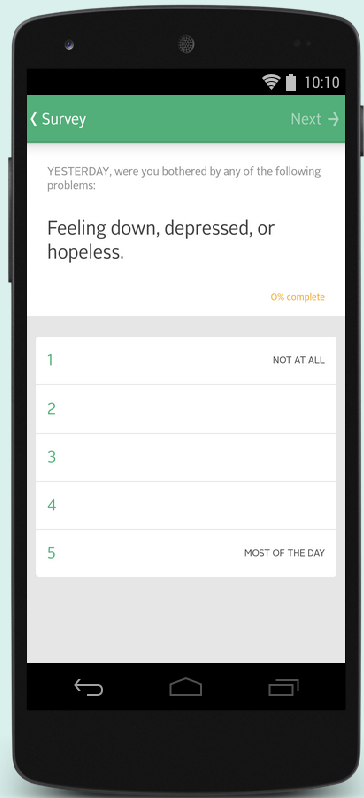 Ginger.io Depression Patient Survey
Ginger.io Depression Patient Survey
The Ginger.io Behavioral Health Program initially enrolled patients who were already engaged in a partial hospitalization program or an intensive outpatient program at the Forsyth Medical Center. In an effort to complement the standard support groups and therapy 3-5 days a week over a 12-month period, Novant Health offers patients the continuous sensing smartphone. Patients download the smart phone app solution from Ginger.io to “connect the dots” between their behavior and their health and “stay in touch with the care team between visits”, according to co-branded patient communications from Novant Health.
The smartphone app actively collects information from the patient about symptoms and medication. Based on the patient’s specific behavioral health condition (e.g., depression), she receives personalized questions to gather a specific set of data. The mobile app also passively gathers data in the background on her mobility, social interaction and sleep patterns. The patient’s active and passive information is then combined and fed into Ginger.io’s analytics engine to identify which patients are in need of intervention and to share that information through an alert with care staff. After receiving a dashboard alert, a licensed mental health professional (e.g. nurse, social worker or case manager) contacts the patient to discuss what is going on in the patient’s life based on her responses and behavior—what Ginger.io refers to as a “behavioral signature”.
Novant Health is already receiving positive feedback and insights from both clinicians and patients.
“Most innovation in Behavioral Healthcare in the past 20 years has been primarily focused on pharmaceutical development,” explains Dr. Todd Clark, Director of Behavioral Health Sciences at Novant Health. “This was necessary for treating patients in the acute phase, but there has only been minor progress related to services detecting mental illness upstream. The Novant Health Innovation Team led by Matt Gymer has created a platform in our healthcare system to leverage the cutting-edge advantage of Ginger.io for our behavioral health population. Ginger.io has revolutionized our ability to connect with patients in real time, even remotely, and allows us to provide patients with the most appropriate and timely care. This not only puts the patient on the most optimal pathway for treatment and recovery, but it also increases the number of treatment options for the patient—rather than the overused default option of the local emergency department. Ginger.io has flexed to meet our system’s particular needs, and our patients have expressed a high degree of engagement with the service.”
Patients appreciate the opportunity to reflect on their mental state and the proactive contact they receive when experiencing challenges in their day-to-day life.
According to one Novant Health patient, “I look forward to the surveys. For the first time in my life I feel that someone truly cares if I live or not. Someone cares how I feel and helps me work through those feelings. I feel I have purpose in my life again.” This is a powerful endorsement from a community in need.
Ginger.io Behavioral Health Program Expansion
Novant Health expanded the program in June to an outpatient drop-in assessment center and mobile crisis unit and then again in September to psych inpatient and psych outpatient clinics. Although these patients come into care during a crisis moment, it is important that they leave with a new tool for ongoing support and empowerment.
Based on qualitative feedback Novant Health from the clinicians and patients using the mobile monitoring solution, care teams have decided to share historical survey responses and behavior patterns with patients through a provider-facing dashboard displaying past data and care alerts. Doctors/Care Managers can share this information with the patient to discuss behavior patterns, life situations, triggers and treatment plans.
Novant Health recently rolled out the Ginger.io technology in their main Psychiatric Clinic in Winston-Salem. Psychiatrists are giving the smartphone app tool to their patients and viewing the dashboard to respond to patients in need. The doctors will also use the information gathered to enrich their conversation with the patient during their office visit.
Novant Health continuously evaluates the value of the program through key quantitative metrics including patient satisfaction and engagement, operational efficiencies and outcomes improvement based on clinically validated measurements such as PHQ-9.
In the future, Novant Health plans to extend the Ginger.io Behavioral Health Program to five other regional hospitals across their health system. The expansion is intended to deliver “a remarkable patient experience,” according to Matt Gymer, Corporate Director of Innovation at Novant Health.
Clinicians are interested in expanding the use of the Ginger.io platform to help them identify patients earlier, understand triggers for their symptoms and proactively provide needed support. This important behavioral health initiative aligns closely with Novant Health’s ability to innovate solutions to deliver proactive care to patients and customize services.
 Motivation for health and wellness,
Motivation for health and wellness,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  personalization for health and wellness in
personalization for health and wellness in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  TeleHealth,
TeleHealth,  shared decision making ehealth
shared decision making ehealth Boston Children's Hospital Monitors Young Patients with Data from Caregivers; Parents, Teachers and Coaches
 September 12, 2014
September 12, 2014  Dr. Eugenia Chan sat patiently waiting for her fidgety first grade patient and her frustrated mother to answer her question. "How was the new medication working to help Janie with her ADHD"? Janie's mom hadn’t had a chance to fill out an ADHD behavior questionnaire in the chaotic waiting area, so she tried to summarize her impressions since their last doctor’s appointment a few months ago. She hadn’t heard specific feedback from Janie’s teacher, and had also forgotten to give the ADHD questionnaire to her teacher so that they would understand how she was doing in school.
Dr. Eugenia Chan sat patiently waiting for her fidgety first grade patient and her frustrated mother to answer her question. "How was the new medication working to help Janie with her ADHD"? Janie's mom hadn’t had a chance to fill out an ADHD behavior questionnaire in the chaotic waiting area, so she tried to summarize her impressions since their last doctor’s appointment a few months ago. She hadn’t heard specific feedback from Janie’s teacher, and had also forgotten to give the ADHD questionnaire to her teacher so that they would understand how she was doing in school.
In 2011, Dr. Chan, MD, MPH, a developmental-behavioral pediatrician and health services researcher in the Division of Developmental Medicine at Boston Children’s Hospital, felt that she needed a better way to monitor her patients and gather insight into how they were doing with their medications and treatment plans. With a grant from the Croll Family Foundation, Dr. Chan collaborated with Dr. Eric Fleegler, MD, MPH, a pediatric emergency medicine physician and health services researcher in the Division of Emergency Medicine at Boston Children’s Hospital, on the development of a new software tool, eDMC (electronic Developmental Medicine Center).
Their goal was to gather and interpret the information from parents and teachers more effectively and gain a more comprehensive view into patient behavior between visits. The doctor determines when the system will email the parents, typically a week or two before the appointment. When the parent receives the email with a link into the software platform, she logs in and answers a set of questions about symptoms, school performance, quality of life, global functioning and improvement since the beginning of the treatment. The parent gives the email addresses of the patient’s teachers and other important observers of the child (e.g., sports coaches, behavioral therapists, tutors) to the clinician to get them set up in the system so they can answer similar questions.
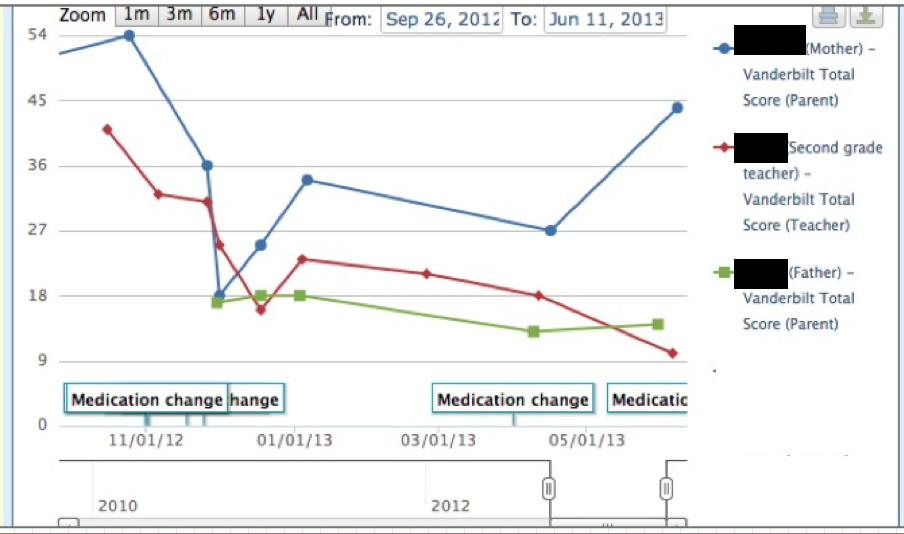 Clinicial InterfaceWith this information, Dr. Chan is able to determine how her patient is doing throughout the day, week and over time. During the visit, she shares this information with her patient and family, points out trends and discusses what has transpired. On the graphs, each line shows data from a different caregiver; parent, teacher and coach. The clinician can also drill down to see specific symptoms and their ratings that are incorporated into a score. With the treatment plan in mind, the clinician evaluates the data and focuses in on any discrepancies to determine what is really happening. This exchange supports her clinical decisions and enables her to participate in shared decision making with her patient and his family.
Clinicial InterfaceWith this information, Dr. Chan is able to determine how her patient is doing throughout the day, week and over time. During the visit, she shares this information with her patient and family, points out trends and discusses what has transpired. On the graphs, each line shows data from a different caregiver; parent, teacher and coach. The clinician can also drill down to see specific symptoms and their ratings that are incorporated into a score. With the treatment plan in mind, the clinician evaluates the data and focuses in on any discrepancies to determine what is really happening. This exchange supports her clinical decisions and enables her to participate in shared decision making with her patient and his family.
“I’ve already started using the system to work with my adolescent patients who want to go off their medications. When I agree to let them try coming off meds, I suggest that we use the questionnaires to monitor results. At the next appointment, patients are often surprised to view parent and teacher ratings and comments, that she was ‘disruptive’ or was ‘unable to pay attention’”, describes Dr. Chan.
Another feature of the platform is the ability to notify the clinician when there is a “red flag” patient problem that may require action (i.e. severe depression). Even though parents are made aware that this is not a real time monitoring system, there is someone responsible for ensuring that clinicians have seen the red flag alert.
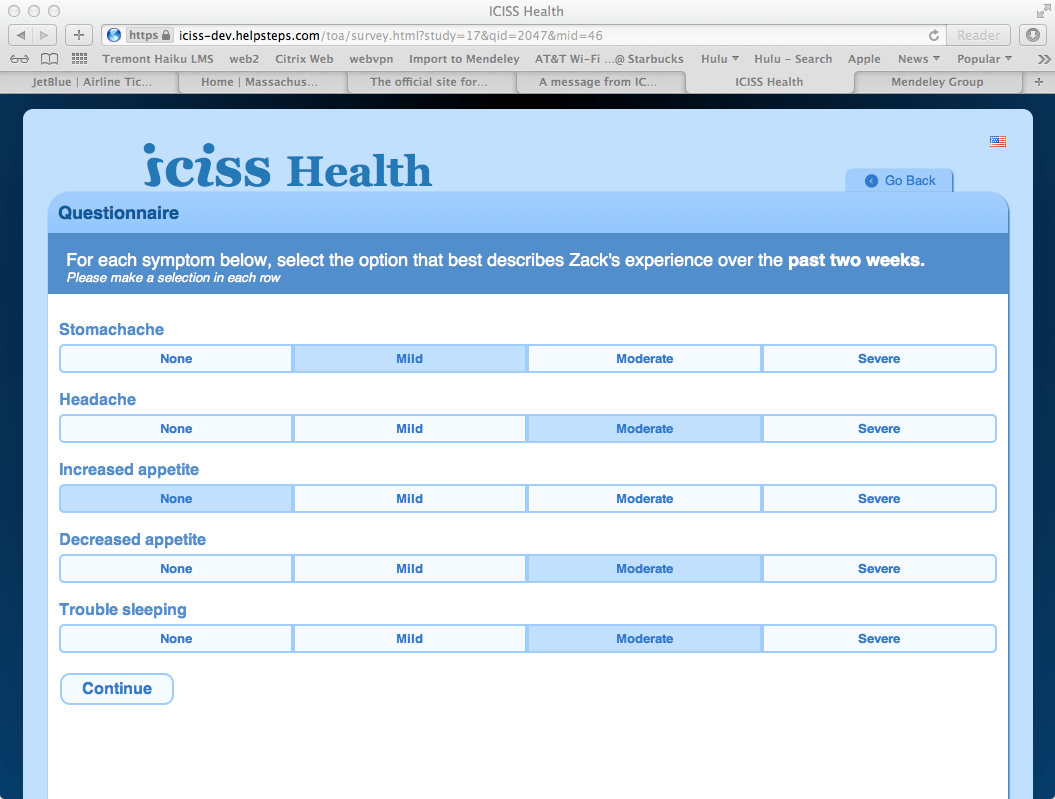 Parent InterfaceSince the program started, over 3,000 pediatric patients have participated. One parent comments on the value that she sees with the system, “it is very easy to use and I like that we save the time at the doctor’s appointment and all of the information is there”. Dr. Fleeger adds that the system “transforms how patients are interacting with their clinicians. At the appointment, the clinician can show them the graphs and tables on the computer to understand where they are and have a fruitful conversation”. Dr. Leonard Rappaport, Chief of the Division of Developmental Medicine at Boston Children’s, says that the platform “is the first major improvement we have made in individualized care for developmental disorders in the past two decades.”
Parent InterfaceSince the program started, over 3,000 pediatric patients have participated. One parent comments on the value that she sees with the system, “it is very easy to use and I like that we save the time at the doctor’s appointment and all of the information is there”. Dr. Fleeger adds that the system “transforms how patients are interacting with their clinicians. At the appointment, the clinician can show them the graphs and tables on the computer to understand where they are and have a fruitful conversation”. Dr. Leonard Rappaport, Chief of the Division of Developmental Medicine at Boston Children’s, says that the platform “is the first major improvement we have made in individualized care for developmental disorders in the past two decades.”
Currently the clinician can copy patient level summary information from the system into the EMR. Although the platform is web- based, Dr. Chan mentioned they were creating a mobile interface for access through smartphones and tablets.
Expanding ICISS Health; More Patients & Populations
In 2012, Dr. Chan and Dr. Fleeger renamed the platform the Integrated Clinical Information Sharing System (ICISS Health) to be more generalized for expansion into other pediatric patient populations.
“We have extended the ICISS Health platform to additional clinics at Boston Children’s that treat patients with ADHD, as well as private practices affiliated with Boston Children’s, and we are expanding into new conditions such as autism, asthma, depression and epilepsy”.
For each new condition, they have convened a cross disciplinary team to define the data that need to be collected to support decisions. “For example, we are working closely with clinicians from the Boston Children’s Autism Center to devise a questionnaire for patients, since there is no standardized set of questions for this patient population” explains Dr. Chan. “For asthma, we would like to invite the school nurse to participate and provide insight into frequency of nurse office visits and rescue medication use by the patient, and whether they used the patient’s asthma action plan.”
The team at Boston Children’s is in the process of collecting information to evaluate the ICISS Health platform impact on patient health outcomes and healthcare utilization and costs. Dr. Chan also mentioned their interest in calculating potential cost savings from the platform by identifying problems early and intervening in time to prevent emergency department visits and hospitalizations.
“As we think about the future of the platform, we are interested in going beyond the electronic questionnaires to capturing and integrating information from devices and mobile applications”, Dr. Chan concludes.
 Motivation for health and wellness,
Motivation for health and wellness,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  family ehealth engagement,
family ehealth engagement,  patient education,
patient education,  patient ehealth engagement,
patient ehealth engagement,  personalization for health and wellness in
personalization for health and wellness in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Consumer Segmentation Health,
Consumer Segmentation Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement
Patient Engagement