Permalink
Permalink Entries in Care access (3)
Providence Health Supercharges Primary Care with AI for Specialist Care Decisions
 September 11, 2024
September 11, 2024 
During the HIMSS AI for Healthcare Forum in Boston, Dr. Eve Cunningham, MD, MBA, GVP, Chief of Virtual Care and Digital Health at Providence Health presented a few AI use cases including an impactful example which empowers PCPs for better care decisions.
Today primary care doctors are pressured to address patient health concerns in an average of 18 minutes with an average of 220,000 data points in the patient’s electronic medical record. With over one in 3 patients referred to a specialist each year, PCPs are tasked with diagnosing the health issue to and making decisions about the need for a specialist.
Barriers to Specialist Care Decision
With vast amounts of patient data that is not clinically organized around context within the patient’s chart, PCPs must spend time pulling together and reviewing relevant information to support the patient’s health problem. Then the PCP must determine if a specialist is needed, and if so which type of specialist.
Given the shortage of primary care doctors and specialists, optimization of the referral process is critical to access to care. However, the referral process today is both inefficient and ineffective causing problems:
- Patient did not need to go to a specialist. (Note: About 20% of patients referred to specialists do not need to see a specialist at all)
- Patient is sent to wrong specialist and/or at inappropriate level of urgency.
- Patient arrives to specialist without any prereferral work-up such as lab, imaging and first-line therapy for a condition.
- Patient has delayed care until there is a specialist appointment
Accelerating Primary Care Referrals
The September issue of NEJM Catalyst’s article on “A Physician-Created Platform to Speed Clinical Decision-Making and Referral Workflow” describes the problem and process that Providence Health has undertaken to conceptualize and build their MedPearl Platform.
“As primary care clinicians struggle to access the expanding base of specialized knowledge and experiences, they attempt to refer patients to specialists, often without the advantage of usable tools at the point of care.”
Developing this needed platform entailed using a “Human- Centered Design approach with a Jobs to Be Done framework, working closely with our clinicians and UX designers”, explains Dr. Cunningham. “We began by asking clinicians how this platform needed to work and look, and got input from 270 clinicians in the design process, which was essential for gaining buy-in”.
MedPearl Platform Built by & for Clinical Care Decisions

Based on clinician’s requirements, Providence built MedPearl as an application within their Epic electronic medical record (EMR) to integrate a digital assistant with clinical knowledge to support primary and urgent care clinicians. MedPearl has “concise, human-authored algorithmic primary and subspecialty care next best actions on over 700 conditions”.
Clinicians utilize MedPearl’s AI algorithms to pull up and review essential clinical information alongside contextualized patient data to see next best actions with what has/hasn’t been done for the patient, empowering clinicians to optimize the “work up” while reducing redundant diagnostics.
Since it can take weeks to months for the patient to get in to see the specialist, the MedPearl platform enables PCPs and urgent care providers to take care of the diagnostics in the interim to optimize the care referral decision. With MedPearl, clinicians can see the testing stream, make sure tests do not need a referral, find the most appropriate specialists and triage the urgency of the specialist appointment based on patient history and diagnostics. Think about what this means for rural health where accessing a specialist is even more challenging.
Providence has designed MedPearl with icons to reduce the clinicians cognitive reading load and provides links to guidelines and QR codes to scan for evidence -based applications.

Clinician Experience with MedPearl
Providence Health has deployed MedPearl across their health system which is available in Epic’s Marketplace.
Dr Cunningham as MedPearl founder comments “Our clinicians tell us that with MedPearl they are spending less time in the EMR, fewer outside work hours and are more productive. To date, we have 7,000 clinician users, making 30,000 searches per month on the MedPearl platform”.
During the initial pilot with 216 participants conducting 14,000 searches, clinicians reported the clinical content helped with clinical decision support: they did not need to refer the patient 20% of time, improved care plan and work-up 72% of the time and changed referral specialty and/or level of urgency 20% of the time.
With MedPearl, clinicians are also realizing better resource efficiency. “We had a challenge with some of our more newly onboarding clinicians overwhelming our Medical Directors with clinical questions and curbside phone calls. The call volume decreased significantly when these clinicians were advised to reference MedPearl first for answers”, shares Dr. Cunningham.
Clinicians often walk through the MedPearl tool with their patients. They review educational content together, discuss the algorithms and use the decision support tools.
Feedback from Clinicans Using MedPearl
After using the MedPearl tool, clinicians commented about the ease of use, quick access to the most essential patient data and benefits of leveraging this patient data for the physician, practice and patient.
“MedPearl provides concise and focused clinical evidence -based summaries, making it easier to quickly access the most relevant information. Its streamlined format saves time and effort, ensuring health professionals can find information without being overwhelmed by unnecessary details”. Medical Director Urgent Care
“The cognitive offloading and reassurance that knowing the Prov approved standard of care has been helpful for me, and I love being able to share it with newer clinicians”. Urgent Care Physician
“The Headache algorithm – perfect example of how to reduce variation in our urgent care practice.” Urgent Care Physician
“With the demand for neurology consultation greatly exceeding the supply of neurologists for the foreseeable future, MedPearl improves access when it has never been more vital.” Chief of Neurology
“MedPearl is a point of care tool we need to augment our clinical acumen and to help drive uniformity of patient care path the best -practice level. This allows primary care physicians to provide more care value, improving diagnostic testing, treatment, and referrals and in opening more specialist access.” Medical Group Director
“Recommendations re: referrals and specific imaging with and without contrast very helpful. Truly has improved physician satisfaction and flow for the day”. Family Medicine Physician
“Contextualization is pretty cool. Makes Pearl useful in multiple ways.. Quick way to see all relevant data about a work up for a particular topic.” Internal Medicine Specialist
“Love the patient experience, engagement and shared decision-making components of this tool.” Practice Senior Director of Operations
“I love the headache algorithm. During a recent appointment, I had a patient point to each symptom that applied to her.” Physician
Future Direction of MedPearl for Health Systems
Dr. Cunningham describes Providence Health’s approach with “feedback and iteration as a core principle by which we drive our MedPearl features roadmap and design. We also push our end users to think beyond the workflow of today, and envision workflow of tomorrow.”
The MedPearl team continues to collaborate with users to gain insight into future enhancements. Specifically, they are focused on these platform innovations:
1. "Expanding contextualization beyond labs, imaging and procedures to further enrich the context aware data aggregation experience"
2. "Adding documentation support features to expedite documentation workflow"
3. "Further refine home page to create a more dynamic experience to delight end users"
4. “Since we believe all workflows will converge on ambient technology, we are preparing ourselves to integrate into ambient workflows. We don’t plan to be the ambient provider, rather we envision ourselves as a clinical intelligence plug-in to further enrich that experience.”
Dr. Cunningham confirms plans to begin “deploying MedPearl to other health systems using EPIC and then Oracle EMRs. We see ourselves as ‘headless’ clinical decision support system that is EMR agnostic and application agnostic. We want to permeate and spread the goodness of MedPearl in a seamless fashion, and meet clinicians and patients where they are“, Dr. Cunningham concludes.
St Lukes Health Expands Patient Access through Integrated Virtual & Hybrid Care Model
 June 25, 2024
June 25, 2024 
During the recent Home & Hybrid Care Virtual Summit 2024, St Lukes Health shared how they have expanded virtual access to support patient care journeys over the past three plus years. It is refreshing to see how St Lukes views virtual as a big front door to their care network, how they have personalized the entrance and experience across more than a half dozen patient programs and how they have invested in an integrated data platform and tools for better care experiences.
Like other health systems, Idaho- based St Lukes Health is addressing today’s healthcare headwinds including staffing challenges, provider burnout, the consumers increased expectations for their healthcare experience, all within the regulatory and reimbursement landscape.
In September 2021, St Lukes Health launched a telehealth program to patients with one of seven low acuity conditions. Since then, their virtual program has expanded to provide patients with immediate care access until they can schedule and see their providers, which may take up to a few months.
“Our team value is that we (virtual care) will be the quickest access to a provider”, explains Abby Losinski, MHA, Director of Telehealth at St Lukes. Abby’s group is part of the Consumer access and experience team.
St Luke Virtual & Hybrid Model
Since late 2021, St Lukes has developed needed processes and infrastructure to successfully expand their virtual program with a centralized virtual support team, virtual command center platform to address incoming patient demand and virtual care patient data integration to support care collaboration and a superior patient experience.
While many health systems launch separate virtual programs to support urgent care, mental health, and chronic conditions, St Lukes centralized team supports many patient populations with virtual care access. They view this virtual interaction as an opportunity to begin a patient relationship.
Several patients targeted by St Lukes for their virtual care program:
- New Patients (December 2021) St Lukes promoted virtual services to welcome patients without a doctor but with an immediate need. During the virtual visit, patients can refill a prescription, get scheduling help and access care support until their appointment. Patients needing a higher level of care are quickly connected with a clinician.
- Urgent Care (May 2022) Patients at St Lukes’ Urgent Care Centers with high wait times are offered a virtual appointment when they meet certain criteria. Patients use their mobile phones for the visit and are urged to stay nearby if point of care testing is required. This gives patients a chance to be seen when there are no available rooms.
- Service Line Extension (January 2023) “We are an extension of any department where patients need same day access” (e.g. primary care, urology, oncology, pediatrics) explains Losinski. “We work with the Medical Directors to build clinical guidelines so that patients are treated the same way whether they are coming in to see a specialist or meeting with our virtual clinician”. Losinski is proud that St Lukes “can offer multi-specialty care from one centralized team”.
- Maternity/New Pregnancy (April 2023) After learning about their pregnancy, patients often have questions and concerns. Instead of waiting for their first appointment which may take 8-10 weeks, patients can meet with a clinician virtually and set up notifications in MyChart to immediately receive information about their maternity care and growing baby. During the virtual visit, patients can get scheduling help and care can be escalated if required.
- Home & Community Access (Sept – December 2023) St Lukes has set up “virtual hubs” enabling patients to connect virtually using digital health tools from a partnership with TytoCare. “We wanted to expand what we can treat virtually because we have new tools. If we can’t see into the ear, we can’t treat it” and the revenue is lost, Losinski explains. St Lukes now offers TytoCare Home devices (e.g. otoscope, stethoscope, throat camera, skin camera) to patients at home and TytoCare Clinic to patients at schools, libraries and workplaces, to capture data for the virtual care team decision support.
St Lukes Virtual Care Access Experience Success
Their virtual program success is achieved through continuous focus on the patient experience. St Lukes has designed their virtual experience from the outside- in and offers patients the bridge into their health system care network.
Here are several success elements that I have noticed to deliver care continuity:
Designed Patient Experience to fit care scenario. Newly pregnant patients are set on the Maternity path, supported by the virtual team with education, testing and virtual visits until their OB appointment. Service Line Extension patients such as oncology may have access to digital tools for remote monitoring with condition education and support until their specialty appointment.
Partnered for Patient Care Coordination. St Lukes’ Consumer access & experience team has built partnerships with different service lines and settings across their network. Patients accessing virtual care at St Lukes needing more care are escalated to these clinical partners within the St Lukes network. St Lukes ensures patient care quality is maintained by using the same clinical guidelines for virtual and in- person care.
Built Integrated Patient Data & Tech Infrastructure. “St Lukes has decided that virtual care can not be this thing that lives outside of the health system”, Losinski emphasizes. St Lukes has invested to integrate and augment patient data (TytoCare devices) enabling clinicians to access information from all clinical interactions and from patients from beyond the walls to deliver better patient care and experiences.
St Lukes Virtual Care Feedback
Through marketing research, St Lukes has learned:
Consumers: The “brand” offering virtual care services really matters. Consumers like that the doctors conducting the virtual visits work for St Lukes and live in the community and appreciate that their PCP can view their virtual visit notes.
Patients: After participating in St Lukes’ virtual services, patients rated the experience an equivalent of 4.9 stars (out of 5). “Thank you for being there when no one else was” shares a patient.
Providers: Clinicians delivering virtual services have a strong provider experience; “appreciate the increased location and schedule flexibility”, “being in the moment for patients” and “getting to work from home”.
St Lukes Virtual Care Direction
Earlier this year, St Lukes launched eVisits, an asynchronous virtual care option. For $29/visit, patients can message a clinician about one of seven symptoms. eVisits are viewed as a virtual care “entry point which affordable and convenient for patients”.
St Lukes will continue expand virtual care access for their patients. “Currently, we are 8am-8pm but we are looking to extend our hours to 24x7” Losinski shared.
It is impressive to see how St Lukes brings patients into their care system through a larger virtual care front door, leverages care partnerships and protocols for consistent patient care quality and empowers care collaboration with integrated data and tools. St Lukes’ virtual care investments and vision enable them to effectively address staffing and consumer expectation challenges while delivering a superior patient and provider care experience.
Providence Health’s Bot Grace engages and guides patients to the digital front door for care
 February 25, 2020
February 25, 2020 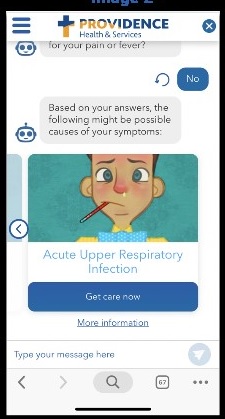 According to the 2019 Accenture Digital Health Consumer Survey, patient’s expectations are increasing for providers to offer digital capabilities. Patients value convenience (appointment times, location) and are increasingly considering “non-traditional” service channels such as retail clinics and virtual care.
According to the 2019 Accenture Digital Health Consumer Survey, patient’s expectations are increasing for providers to offer digital capabilities. Patients value convenience (appointment times, location) and are increasingly considering “non-traditional” service channels such as retail clinics and virtual care.
Providence Health’s Innovation team continuously monitors these trends to identify ways to deliver a better patient care experience. “With the tremendous growth of chatbots and voice assistants, we decided to develop a virtual health assistant and begin to understand how to support the patients in their search for care”, explains Maryam Gholami, Chief Product Officer at Digital Innovations, Providence Health.
In fall 2018, Washington State based Providence St Joseph started developing and testing Grace, a chatbot which asks the patient about their symptoms and based on their location, time of the day and scope of services provided in various care options (virtual, clinics, or At Home) directs them to the best care. Eventually Grace was enhanced to also address frequently asked questions by patients.
Since the healthcare system is complex for consumers to navigate, Providence Health designed their digital tool to provide answers and guidance to help the patient find the right care and make the best care decisions. For example, a consumer may not know which modality of care to use (e.g. Emergency Room. Urgent Care, Retail Clinic, Virtual/Telehealth) or what symptoms trigger an immediate visit.
On the consumer side, Providence Health wants to stay aligned with their patient’s increasing expectations for service on demand. Consumers are already using digital assistants for shopping, banking and travel 24x7.
“From a business perspective, we want to provide accessible, convenient and affordable care. Therefore, we need to improve operational efficiency, free-up professional caregiver capacity for the right care and tasks, while increasing the care options and quality for consumers. We want to have our virtual health assistant take on the administrative tasks so that our clinical staff can focus on patient care. For example, Grace conducts a virtual patient intake to schedule a visit, collecting information such as reason for the visit, demographics, insurance and payment details”, explains Maryam. “This digital health assistant also assesses the best modality of care based on patient’s input and availability of care, matching the right resource to meet each patient’s needs. With this type of service navigation, Providence Health can ensure that the required license level is designated for the visit, reducing care cost and ensuring availability of providers for the appropriate level of care. Healthcare is supply-constrained, so this is a very important value.”
Patient Experience with Grace Bot
Providence Health has worked closely with the patients to design the Grace bot. Here is a look into the patient experience.
Patient Patricia who lives in Washington State, types her symptoms into Google to figure out what she has and where she can get care. Within her search results, Patricia sees a Providence Health website link and then meets Grace, a pop- up text chatbot ready to help her.
The Grace bot helps Patricia in two important ways:
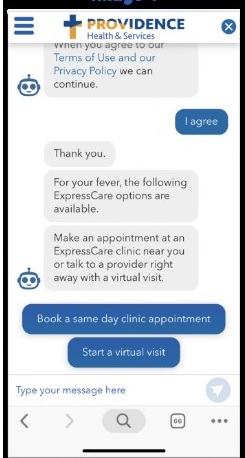
1. Care Navigation: Given that Patricia needs “same day care” and has a low acuity health problem, she types into the Grace bot that she has a fever and sees that Grace has recommended a virtual visit or a same day clinic appointment. Patricia provides her zip code, chooses the clinic near her house and schedules an appointment for 7 PM that evening.
2. Customer Service/Concierge: Patricia has questions about whether her insurance is accepted and types in “what insurance do you take?” Grace provides a list of insurance options. Patricia can also ask for information to read about her health problem before her visit.
Patient Experience with Grace Bot
The Grace bot was designed for patients by patients. Throughout the development process, the product team at Providence Health worked closely with patients to understand the “tasks they were trying to complete” and defined how Grace needed to guide them through these steps. During testing, the team monitored where patients dropped off and tuned the messages to “optimize” their care journey.
“We are digging into the questions that our customers ask so that we can improve our knowledge base. This enables Grace to better respond to our patient questions”, Maryam explains.
With ongoing patient feedback, Providence Health has identified and has been addressing several areas to improve the patient experience.
Chatbot Persona: Maryam shares that “we used emojis to make the digital interaction more casual and friendly. Our patients did not like the emojis because they felt emojis do not convey trust which is essential when communicating health information. Patients also needed to feel comfortable that the responses and recommendations were not coming from a human. We are working on the right persona for Grace and defining the best interaction”.
Chatbot Behavior: Providence Health’s product team is determining when Grace needs to confirm information with the patient so that it accurately reflects her needs. There is a fine line between repeating back to be sure and being annoying to the patient who is looking to quickly complete her task (e.g. set up a visit). However, there is a risk of sending the patient to a modality that does not meet her needs (i.e. she needs to see a doctor and not an RN). “We need to understand the clinical operations from end to end so that we can define the business rules to successfully guide the patient interaction”, Maryam comments.
Consumer Adoption: Some patients are pleasantly surprised about what the Grace chatbot can do for them. Others may not understand what to ask her. Health organizations will need to educate consumers on the types of questions to ask so that patients can gain the most value when engaging with the bot.
Provider Adoption: Providence Health is working on enabling the Grace bot to support virtual care. Grace can engage with the patient to capture information prior to the telehealth visit. However, we need to ensure that this is designed and implemented in such a way that clinicians can properly review all of the information captured before the visit begins and that we are not increasing provider burn-out. It needs to improve the experience for both patients and providers.
Patient Representative Experience: When the Grace bot “hands off” the patient for the scheduled visit or for further follow up, it is important that the representative knows that patient just engaged with the Grace chatbot, has the context and the information already collected and can address the patient accordingly.
Chatbot Success Evaluation
Maryam shares some key success measures for the Grace bot. “We currently know that over 42% of our patients who engage with Grace get answers to their questions or get help navigating to the right modality of care. 18% of these engagements result in completion of appointments booked with one of our ExpressCare Clinics (Urgent Care). We are also learning which questions Grace doesn’t know how to answer or which tasks she can’t currently complete. This learning is very important to help us with our future product direction and iterations”.
Patients interacting with Grace can navigate to Providence Health’s ExpressCare options based on a chief complaint or use a symptom checker before choosing recommended ExpressCare options. Providence Health is seeing a 90% accuracy rate for patients that have been directed to ExpressCare from the patient’s chief complaint.
According to Maryam, there are weekly meetings with the product analytics team to understand how patients are using Grace so that they can enhance the patient experience. “We measure every interaction in the funnel to understand if we’ve helped users complete their tasks. Some of these measure include # of click rates, # of patients questions answered, # of appointments booked, # of visits completed along with type of visits, and chatbot engagement when the customer support center is closed”, describes Maryam.
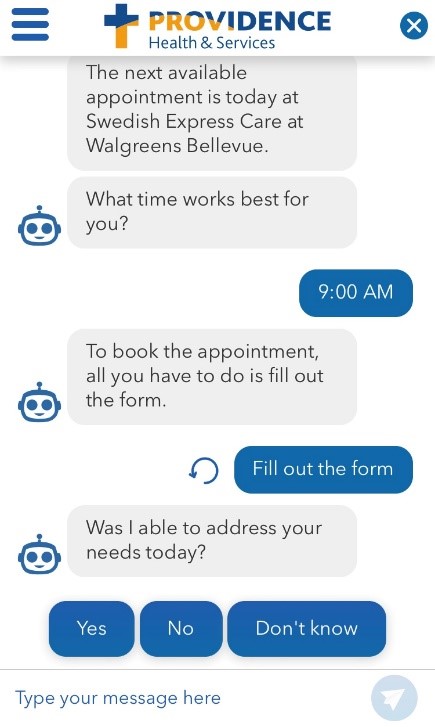 At the end of each interaction, Grace asks the patient if he is satisfied with the task – “Was I able to address your needs today”? According to Maryam, about 40% indicate that the Grace bot met their needs. Providence Health is closely listening to patient feedback to increase the satisfaction percentage.
At the end of each interaction, Grace asks the patient if he is satisfied with the task – “Was I able to address your needs today”? According to Maryam, about 40% indicate that the Grace bot met their needs. Providence Health is closely listening to patient feedback to increase the satisfaction percentage.
Providence Health has received insightful patient feedback about the Grace bot experience:
“This was the first time I’ve seen something like that, I thought it was extremely helpful. It asked a lot of good questions to get me the right help.”
“I felt like it was really easy to get an appointment. Very quick automated responses got me to the right place.”
“I thought it was excellent. I research a lot of my own health issues, so I’m excited about this. Anything that can help me learn about my symptoms and what to do about them, I’m excited for it.”
“For me, it was kind of cold. If it could change the wording to make it more human it would be better. I’d prefer a more human touch to it. I think in this field personality is important, so work on making it more warm, caring, and friendly.”
Future Plans with Grace:
Providence Health is committed to enhance the Grace virtual health assistant experience for patients by:
Expanding the patient journey: Currently, Grace is available more in the discovery phase, when patients are searching for care options. “Next, we are incorporating Grace into the Virtual waiting room to gather intake information before the patient participates in the telehealth visit. Our goal is to have Grace available when/where appropriate to help consumers navigation through health journey”, Maryam adds. “We are looking to move beyond low acuity to helping patients find and book PCP and Specialty appointments”.
Increasing the personalization: While Grace currently does some personalization based on consumer’s location, time and symptoms. Providence Health believes there is still a great deal of opportunity to leverage various sources of data including patient records. They will proceed carefully given the consumers’ data security and privacy needs.
Improving the High Tech & High Touch Collaboration: “We view our virtual assistant as an augmentation tool for our professional caregivers. We are working on creating a warm hand off to human caregivers with the conversation context. We are designing these tools so that based on consumer’s choice, human caregivers can step in to assist our patients”, explains Maryam.
Providence Health’s clinical and business leaders believe that offering these virtual health assistants are essential to delivering the best care experience for the patient, today and in the future.
“We are levering technology to connect the consumers to the right place for care with the right service and providers at the right time. AI is going to help us to improve the seamless experience.” Thanh Nguyen, Executive Director and Chief Clinical Officer of Express Care
“AI-powered virtual assistants will have a significant impact on healthcare by engaging consumers through voice/chat, a more natural way of interaction, and by intelligently automating mundane tasks and simplifying complex ones at scale.” Aaron Martin, EVP, Chief Digital Officer
 Permalink
Permalink  chatbot,
chatbot,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness in
educating consumers about health and wellness in  AI,
AI,  Care access,
Care access,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision support,
Decision support,  Mobile Health,
Mobile Health,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Patient Journey,
Patient Journey,  TeleHealth,
TeleHealth,  Virtual Health Assistant,
Virtual Health Assistant,  digital health,
digital health,  patient health education
patient health education