It all started with a simple question one day, and grew into a trusted health relationship a few short months later. Sarah was very busy at work that crisp fall morning and had only a few minutes to log in and ask about her daughter’s diabetes medication. Sarah was comforted by the response and a bit intrigued when her Health Assistant Harriet introduced herself and explained that she is a resource to help her and her family with any of her health questions or concerns. They began a conversation about her daughter’s condition and a trusted relationship began.
Later that week Harriet made a follow up call to see if Sarah was able to pick up her daughter’s medication and asked how everything was going. Sarah mentioned that she finally got her daughter’s pills and confided that she was completely overwhelmed. Sarah shared that she was recently diagnosed with breast cancer and that her husband was often unavailable as he traveled constantly for work. She explained that she had a hard time getting to her treatments. After their call, Harriet explored and evaluated resources, and scheduled transportation to help Sarah get to her next appointment. Harriet put the appointment confirmation into Sarah’s patient portal and set up a reminder, including date and time, about the ride to her next treatment.
This may sound like fiction in the current healthcare environment, where services are siloed and patients are burdened with making their own decisions around healthcare – often complex and costly. Sarah is relieved to have this service today. She first learned from her employer about the Accolade platform and health advisor service last summer. It wasn’t until she reached out with a simple question to her health assistant that Sarah experienced the true value of having a healthcare advisor on her side.
A 2016 Harris Poll reveals that 84% of working families placed a value on having a single, trusted resource to help support their healthcare needs. Busy families have limited time and resources so they appreciate having one place to go to help them understand their options and sort through their healthcare decisions.
Personalized Patient Experience

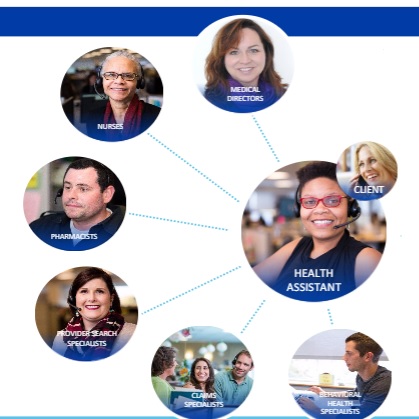
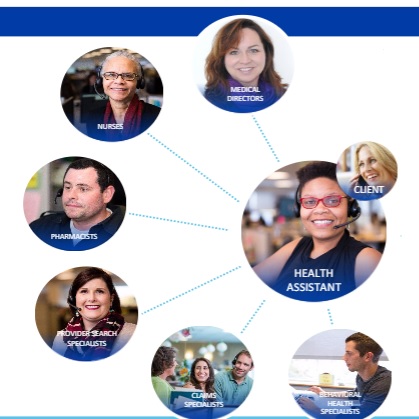
With the Accolade Health Assistant as the single point of contact for her family, Sarah is able to reach out to Harriet for guidance all along her and her family’s healthcare journeys. Accolade integrates high tech and high touch to deliver a superior patient experience with lower healthcare costs.
Accolade Health Assistant Harriet accesses the Accolade platform to interact with and personalize her support for Sarah:
Preferred Communication: Harriet engages with Sarah and her family based on their communication preferences. Sarah likes phone calls and email through the Accolade online portal. Sarah’s husband Sam prefers secure text messages since he can send quick messages and follow up later during his business trips.
Personalized & Proactive Experience: Harriet’s interactions with Sarah are driven by rich patient profile information, which contains contextual information, social determinants of health and service utilization. Sarah and her family’s profiles are updated with data collected over time and more than 150 data feeds integrated into the Accolade platform. The HIPAA-certified approach creates profiles that are continuously analyzed through sophisticated algorithms and health assistant reviews, which allow for personalized conversations around individual health needs, care gaps and obstacles.
A recent Accolade platform trigger prompts Harriet to reach out to Sarah’s husband Sam when she notices that he is still refilling this pain medication many weeks after his knee surgery. Harriet sent a text to Sam to inquire about his knee surgery. After a text exchange, Harriett suggested that he see his doctor to discuss his persistent pain.
Patient Education & Connected Health: Sarah and her family can access educational information and recommended health apps. Before Sarah’s husband knee operation, Health Assistant Harriet texted Sam with a link to a video and suggested questions to prepare for his surgery and provider discussion.
When Harriett spoke with Sarah about her daughter’s diabetes appointment and care plan, Harriet informed Sarah about the Livongo mobile diabetes application available through her employer’s health plan. Together, they review the Livongo app, which can help Sarah and her daughter better track and manage her diabetes. With Accolade and Livongo, Sarah is able to share information from the mobile app with her daughter’s doctor, giving him insight into her problems with controlling her A1C levels.
Continuous Connection to Clinical Resources and Support: Harriett asked Sarah if she would like to speak with an oncology nurse to help prepare her for her upcoming oncologist appointment. Margaret, an Accolade Clinical Health Assistant and RN, joined them on the line and offered empathetic support by asking more about Sarah’s diagnosis, where she was in her care plan with her doctor, whether she had a support network and what was planned for her next appointment. Margaret provided Sarah with questions to ask her oncologist and recommended a follow-up discussion.
Intelligent Engagement: Harriet and her Health Assistant team are continuously alerted by the Accolade platform. On an ongoing basis Accolade gathers, aggregates and models de-identified data to trigger alerts and guide Health Assistants in further personalizing their interactions with their clients. Health Assistants are prompted to ask questions about health behaviors and emerging symptoms, applying specialized training and skillset.
Patient Experience Success Measures:
Paul Csigi, Director of Benefits at Philadelphia- based Temple University Health System (TUHS), rolled out the Accolade solution in 2015 and has over 7,000 employees on the platform today. “So much of healthcare is getting people to the right place at the right time. Accolade has created an experience where our employees build a relationship with an assistant that gives them what they need, when they need it. Accolade takes a single problem that the patient has called in about and creates a relationship to support the family on an ongoing basis. With all of the information about our employees, Accolade addresses the whole person, connects the patient with clinical resources, and continues to reach out. This helps treat our employees sooner, which is less expensive for our organization.”
In addition to financial measures, TUHS monitors qualitative feedback from employees. With the Accolade platform outreach (phone or online), TUHS is able to capture the patient’s experience engaging with their Accolade Health Assistant:
“I'd like to thank Temple for the Accolade program. We have been going through some really tough times…..my health assistants have been a big support and a big help to my family in helping to guide us to the right doctors to help with family issues and illnesses. I really appreciate this program. Without it, I'd really be lost.”
“It is great having that person who is able to explain things to you and walk you through the process….It makes navigating the current health care world so much easier and less stressful. That is exactly what you need when you are dealing with a health care issue.”
“I spoke with my health assistant and then with the nurse, and they were incredibly helpful. They spent a lot of time on the phone with me, helping me understand how to navigate the system, and what questions to ask.”
“He [Clinical Health Assistant] made this very difficult hospitalization for my husband an easier journey. Without him, I wouldn't have been able to accomplish many things….I am extremely grateful.”
Patient Experience Journey
With two years of the Accolade solution under their belt, Paul Csigi and his team are considering new ways to support TUHS employees. “I have an employee population with diabetes and heart disease. I am interested in learning more about Accolade’s partnerships to bring patient data into the platform to support these populations.” Csigi sees the benefit of bringing in data from patient devices and smart applications. Integrating this data with the patient’s medical record gives new insights to Accolade Health Assistants, empowering them to deliver even better support and drive improved outcomes.
 consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  mobile health and wellness texting,
mobile health and wellness texting,  online health and wellness coaching,
online health and wellness coaching,  online health and wellness support,
online health and wellness support,  self- management health tools in
self- management health tools in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care Coordination,
Care Coordination,  Care collaboration,
Care collaboration,  Caregiver digital health,
Caregiver digital health,  Connected Health,
Connected Health,  Consumer Segmentation Health,
Consumer Segmentation Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Employee Engagement Health & Wellness,
Employee Engagement Health & Wellness,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Engagement,
Patient Engagement,  Patient Portal,
Patient Portal,  Population health management,
Population health management,  eHealth Channel Strategy,
eHealth Channel Strategy,  online coaching,
online coaching,  shared decision making ehealth
shared decision making ehealth