The National Cancer Institute reports 2017 U.S. cancer care expenditures were $147+ billion, with anticipated increases from our aging population.
The National Cancer Institute reports 2017 U.S. cancer care expenditures were $147+ billion, with anticipated increases from our aging population.
According to Deloitte’s report in Evidence Based Oncology ( The American Journal of Managed Care publication), many organizations are exploring ways to control costs and enhance care quality for oncology patients (e.g. Patient Centered Medical Homes, CMS’ Oncology Care Model).
With many different types of cancer and treatment options, each patient embarks on a personal care journey.
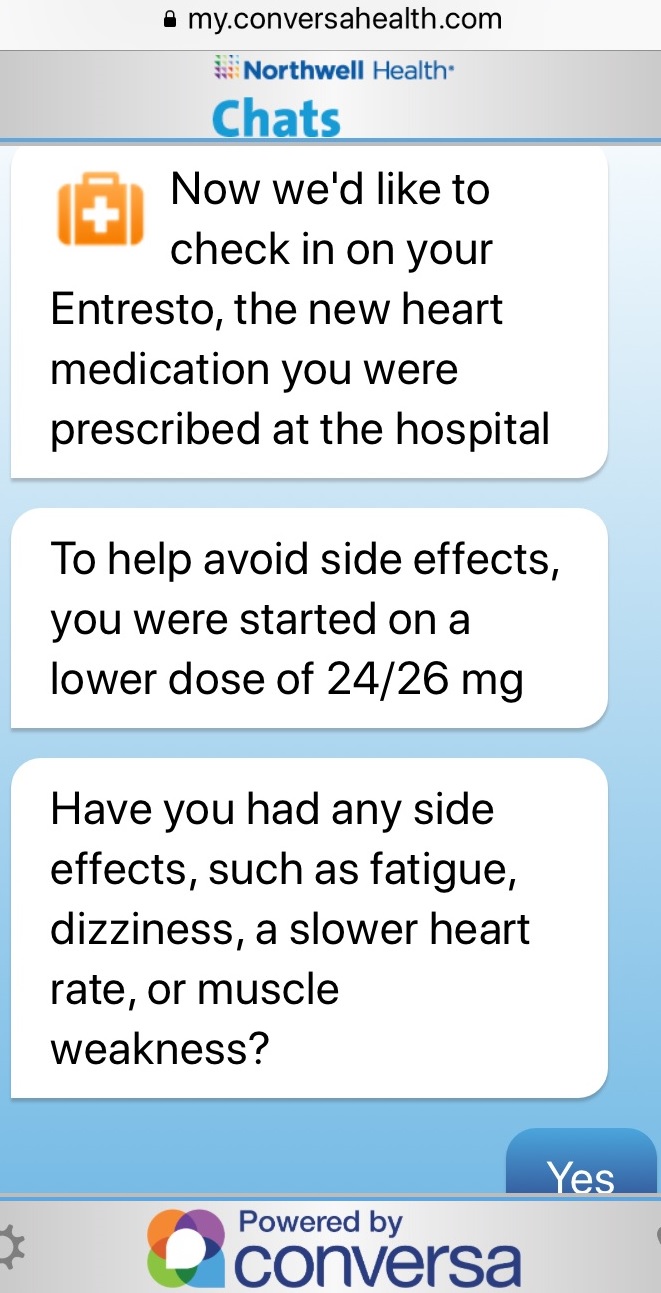
Oncology patients often experience a long journey. Although some steps entail engaging with care staff at a hospital or clinic, most of the time patients are challenged with managing their disease on a daily basis away from the health system.
Healthcare organizations need to closely monitor oncology patients to determine when care and support is required. To be proactive and stay aligned with patient needs, health systems must collect patient information (e.g. Patient Reported Outcomes/PROMs, Patient reported experiences/PREMs). This patient information can guide the care team to intervene, reducing hospitalizations and costs.
Northwestern Medicine’s Oncology Program
“We wanted to take a holistic approach with our oncology patients; mind, body and spirit”, explains Dr. Martha L. Twaddle MD FACP FAAHPM HMDC, Medical Director - Palliative Medicine & Supportive Care, Northwestern Medicine, Lake Forest North Region. “We wanted to help our patients navigate their oncology journey, figure out their new normal and participate in their care”.
“A few years ago, we successfully used a patient engagement care tool with our palliative patients. Our palliative team is embedded within Oncology. Eighteen months ago, we introduced this telehealth type of application to our oncology patients. We felt it would be valuable to extend TapCloud to our general oncology patients because we had seen such a positive response using it for those with high symptom burden and advance disease. We believe many patients and caregivers will benefit from having this tool available to use”.
Patient Experience
How does TapCloud support the oncology patient? What is the patient experience?
 Last month, Robert (not his real name), a 77 year old patient was diagnosed with prostate cancer. Dr. Twaddle and her staff worked closely with Robert through the onboarding process to provide an overview, demonstrate how to use TapCloud, help him download the TapCloud app onto his phone and iPad and discuss what symptoms they will manage to personalize the app for his specific condition.
Last month, Robert (not his real name), a 77 year old patient was diagnosed with prostate cancer. Dr. Twaddle and her staff worked closely with Robert through the onboarding process to provide an overview, demonstrate how to use TapCloud, help him download the TapCloud app onto his phone and iPad and discuss what symptoms they will manage to personalize the app for his specific condition.
The Nurse Coordinator explained “Robert, with this tool (TapCloud), we can think about you when you are not in front of us, get a sense of how you are doing and that we are on the same page”. Robert was relieved to get a message from his Nurse Coordinator confirming that she can see Robert listed on the dashboard to keep a close eye on him.
Most of Dr. Twaddle’s seventy active patients using the TapCloud App are in their 60s and 70s, with a few in their 80s and 90s.
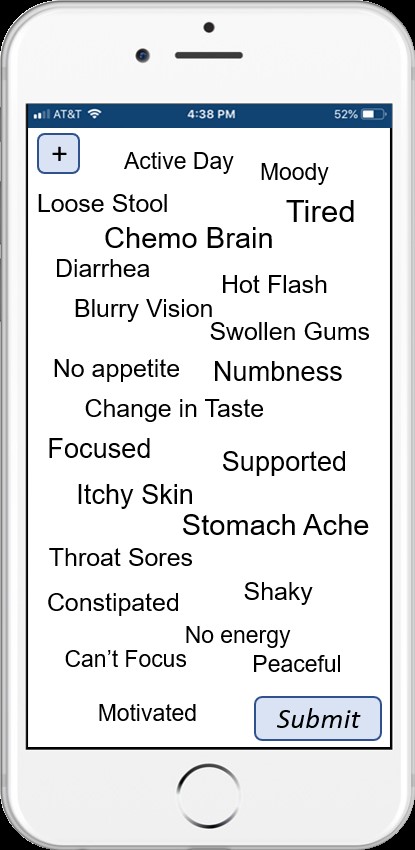
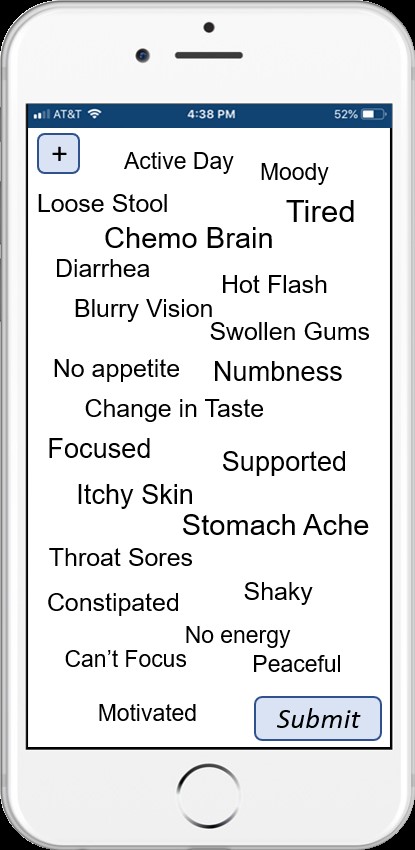
Through the TapCloud app Care Plan, patients like Robert are asked a set of questions. How are you feeling today compared with yesterday? Which of these meds are you taking? Which symptoms are you experiencing today? Symptoms that were selected the prior day are displayed bold. Patients can add symptom(s) which typically takes less than a minute to provide this critical information.
Symptom tracking is made easy by using a word cloud. Each day, the patient sees a personalized word cloud containing symptoms. This personalized symptom cloud incorporates his condition and medications and his list is continuously enhanced from machine learning. TapCloud’s predictive symptoms cover 100+ conditions and 14,000+ side effects. The patient simply touches those symptoms he is noticing. Additionally, he views personalized education based on his journey stage (e.g. tips for managing chemo side effects) and what he is experiencing. He can also upload this biometric information (e.g. vitals, etc.).
How has Northwestern Medicine used the TapCloud tool to deliver better care to Oncology Patients?
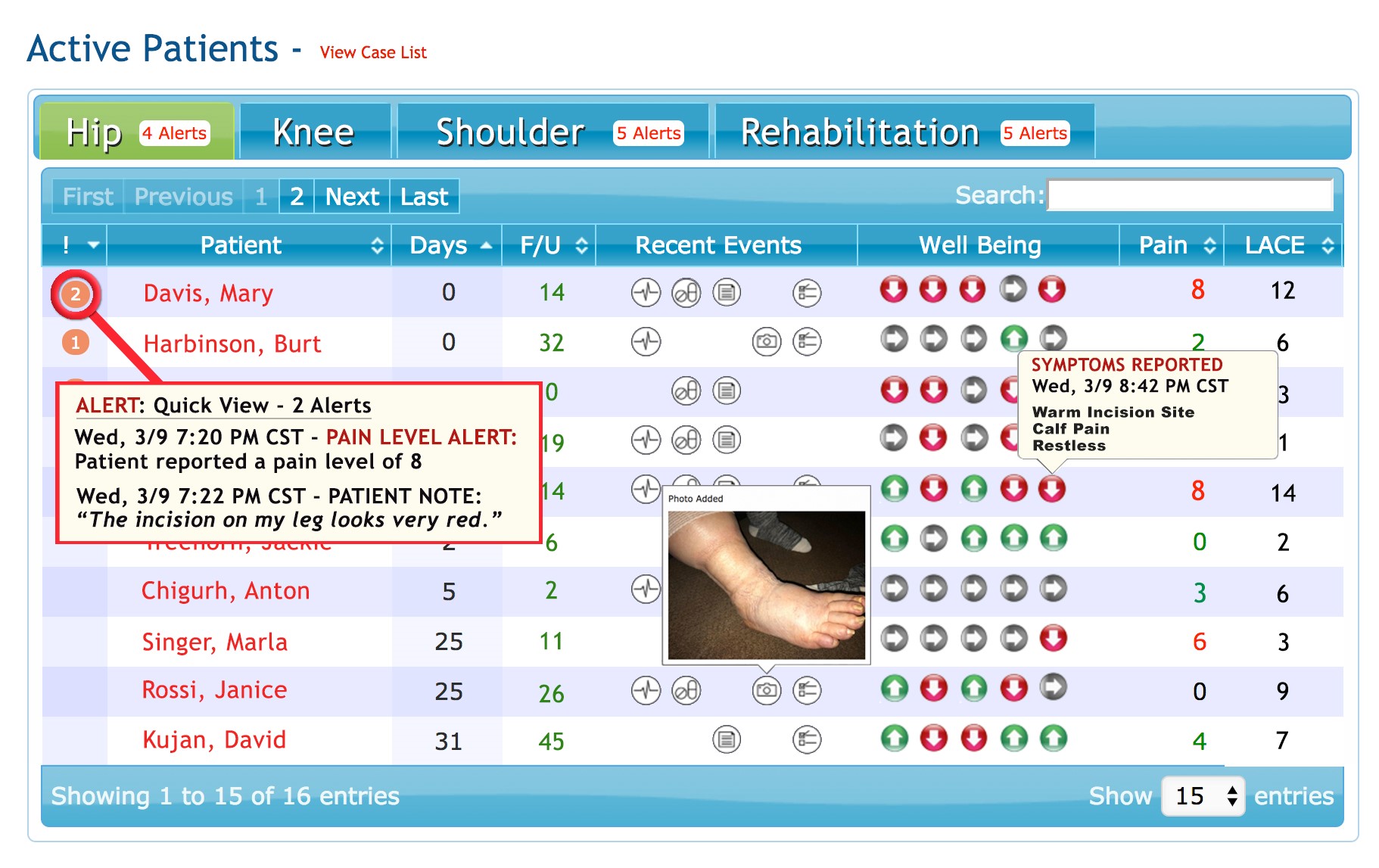
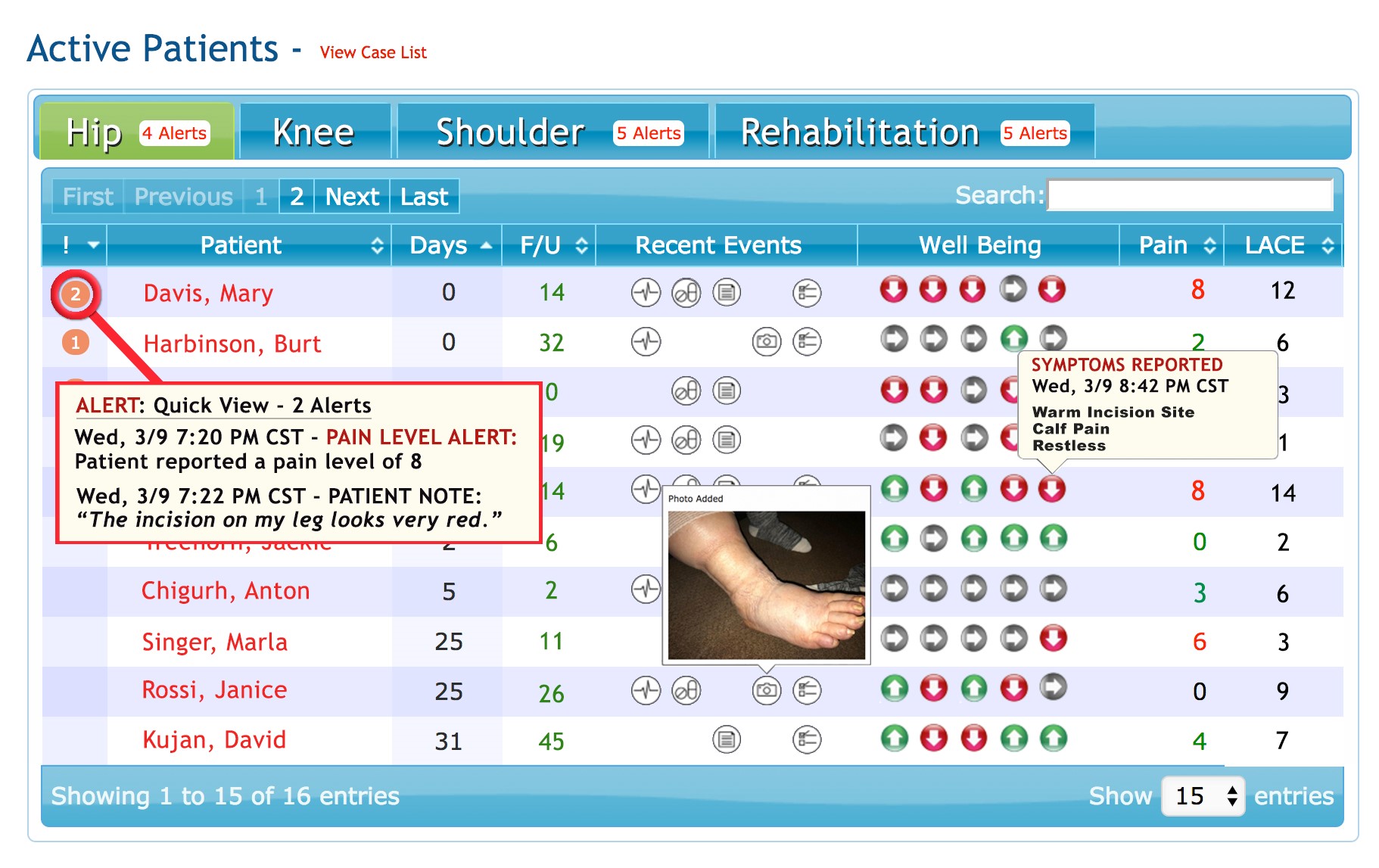 Dashboard displays demo data only
Dashboard displays demo data only
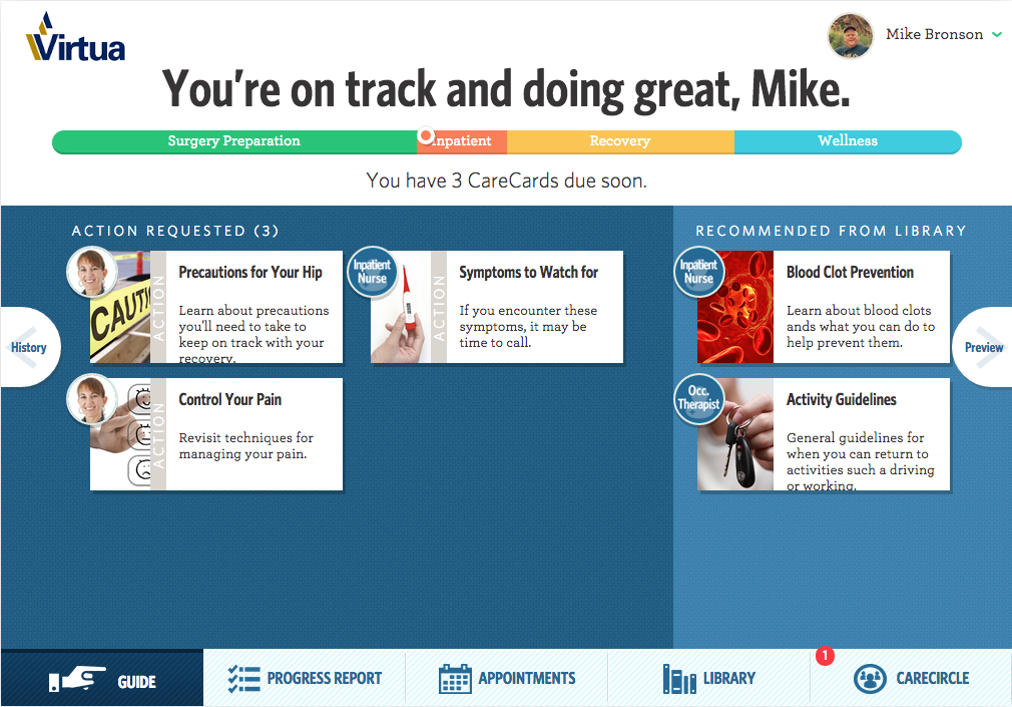
- Prioritize Patient Outreach. The TapCloud platform analyzes all the patient clinical and self- reported data in real time. Using advanced algorithms, patients with a clinical need are identified and alerts are sent to the care team. Patients are prioritized based on alerts, severity and risk. Nurses use the TapCloud Triage Dashboard to efficiently track, monitor and respond to patients requiring an intervention. Nurses can drill down on a specific patient to see how many days since check in, recent events (e.g. vitals, medication usage), pain and anxiety levels.
- Intervene on specific symptoms: Instead of “fishing” for information about how a patient is feeling or having the patient end up in the ER, Nurse Terri can call the patient and say “I've noticed that you've had increased pain the past 2 days…”. TapCloud can also be set up to send alerts for symptoms associated with a patient’s treatment. Patients can send a picture within the TapCloud app with a secure message about their concern.
- In the Patient’s Words: “We had one patient who didn’t feel pain but entered ‘yuk’. He selected that to communicate in his words what he was feeling. One of the features that I really like is journaling. A patient may share that today he is ‘discouraged by his illness’. Although he does not expect us to respond, it gives us insight into how he is doing and the support that he may need from us”, shares Dr. Twaddle.
- Stay Connected with patients who do not come in regularly: When patients are going through infusion treatment, Dr. Twaddle explained that her team sees them on a frequent basis. “However, when our patients are on oral chemo, we feel that TapCloud is especially valuable to give us a window into their experience. We risk losing them because they cannot tolerate the medications and stop without communicating to us.”
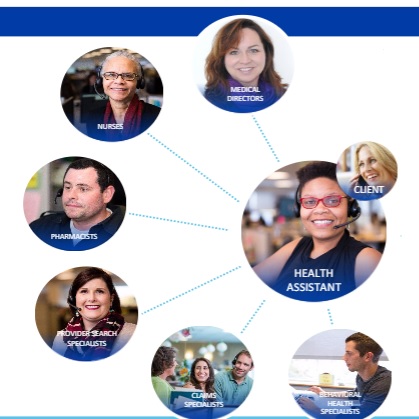
- Address Patient Needs with Right Resource: When patients are not in the Clinic or Hospital, it is important to understand what they need. “We may see in a patient’s journaling that she is feeling afraid which is not physical but may be best addressed through our psych- social resource. Or a patient may be ‘running out of her medication’ or ‘checking in on an upcoming appointment’, which can be managed by our Nurse Coordinator."
Measuring Success
Dr. Twaddle uses a set of quantitative and qualitative measures to evaluate the success for the TapCloud solution for oncology patients including:
1) Patient Engagement. How involved are patients in participating in their care? How often did they check in with the app? Which symptoms are most common? What are the new symptoms that have been added by the patient?
2) Improved symptom management. Was pain successfully controlled (e.g. pain scores, pain direction)? Were negative symptoms (e.g. fatigue, bloated, shoulder pain) managed in a timely and effective manner?
3) Cost reduction. How much money was saved by avoiding ER through interventions on symptoms? “When one of our cancer patient ends up in the ER, we explain that we may be able to help avoid the admission with a check in on the TapCloud tool. We had one patient with a side effect that we could have spotted and intervened since it was dangerous for her”.
“We have found that TapCloud is helpful both with cancer patients who have declining function (e.g. pancreatic, advanced lung, brain tumor) and with those that may be curable (e.g. head & neck, breast)", shares Dr. Twaddle.
AMITA Health’s Program will leverage TapCloud
AMITA Health, one of Illinois’s largest health systems is in the process of planning their program which will use TapCloud.
“When I first heard about TapCloud, I was on board immediately”, explains Dr. Robert O. Maganini, Breast Cancer Specialist at AMITA Health. “We have a compliance problem with our breast cancer patients. Although the hormone therapy treatment (e.g. Tamoxifen, Class Aromatase inhibitor) is for five years, some patients will stop after two years because of the side effects. Our working theory is if we have insights into where these patients struggle and when, we can do more aggressive interventions instead of waiting for their next appointment”.
“Our plan is to offer TapCloud to all 200 patients who want to use it, from newly diagnosed to those in year two when we experience a drop in treatment adherence”. After describing his patient population – mostly women 40-75 years old, Dr. Maganini expects a high opt- in rate since it is “ideal for them because it enables faster and more convenient access to their provider”.
Like Dr. Twaddle, Dr. Maganini is planning to use a patient- centric approach when introducing TapCloud, ensuring that patients understand why they are using TapCloud, how to use it, and when to use it.
Dr. Maganini plans to introduce TapCloud to patients at the time of diagnosis. Nurses (e.g. NPs, Navigators) will get patients set up and show them how to use the digital health application. “Since surgery is typically the first step, we plan to use as a follow up with discharge instructions. For those in going through chemo treatments, we will monitor their symptoms. We want to get our patients accustomed to using TapCloud and then they will be using it for the long run with hormone therapy”.
As part of the planning process, Dr. Maganini is working with his team to define the list of side effects including the words that these patients use to describe them. He is leveraging his own and his nursing staff’s patient experiences to devise the TapCloud symptom list in “patient speak”. This is helpful to patients who often struggle to describe their symptoms and feelings.
From this program, Dr. Managini expects to learn about the top side effects, interventions and the effectiveness of the interventions. He will be looking at different success factors – “increase in the therapy completion (3, 4, 5 years) and longer term (beyond the 2 years) hopefully a decrease in mortality rate and reoccurrence”.
“With a program showing demonstrative effectiveness, we envision scaling this to the AMITA Health 2.0, 19 hospitals”, concludes Dr. Managini.
 Permalink
Permalink  consumer generated health and wellness content,
consumer generated health and wellness content,  mobile health and wellness texting,
mobile health and wellness texting,  patient education,
patient education,  patient engagement,
patient engagement,  patient experience,
patient experience,  patient journey,
patient journey,  patient reported experience measures,
patient reported experience measures,  patient reported outcome measures,
patient reported outcome measures,  personalization for health and wellness in
personalization for health and wellness in  AI consumer engagement,
AI consumer engagement,  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care collaboration,
Care collaboration,  Caregiver digital health,
Caregiver digital health,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  Population Health,
Population Health,  TeleHealth,
TeleHealth,  TeleMedicine,
TeleMedicine,  patient health education,
patient health education,  shared decision making ehealth
shared decision making ehealth