Health systems today are facing a perfect storm with increasing demand from an aging and sicker population and decreasing supply of physicians to support these patients.
AAMC’s (Association of American Medical Colleges) latest report (2024) projects the United States will “face a physician shortage of up to 86,000 physicians by 2036.” In some specialties, like behavioral health and dermatology, the wait for a new patient to see a physician can be weeks to months, depending on the system, type of problem and expertise needed.
To address this care access problem, Ochsner has been investing in AI tools to drive patient access with intelligent triaging to connect them with providers at the right care setting. For every patient, it is critical to get to the right provider 100% of the time.
Recently, Ochsner incorporated AI guided eConsults to empower the patient’s Primary Care Physician with insights from the specialist until the patient can be seen.
Ochsner’s two AI- driven tools for better patient care:
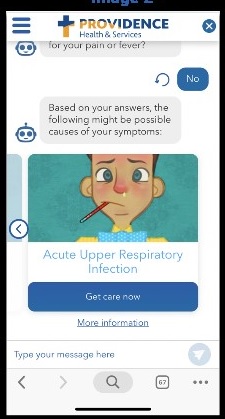
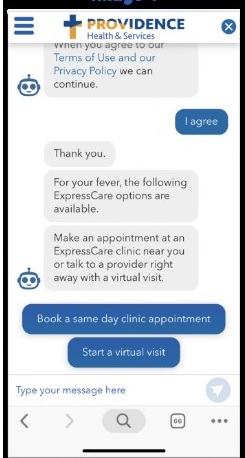
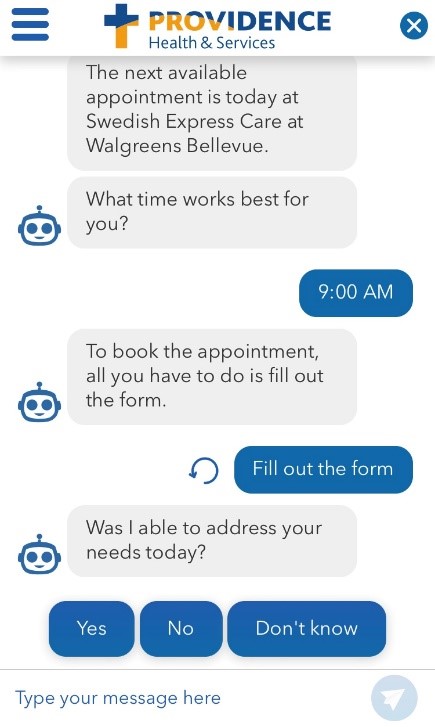
1. Intelligent triaging uses the Clearstep Smart Access chatbot to guide patient navigation.
Since Q2 2024, Ochsner’s use of Chatbots and Large Language Models (LLMs) has offered an excellent way to guide patients to the right level of care, while also enabling the healthcare system to dynamically meet the demand.
When a patient goes to Ochsner’s website and types into the Clearstep Smart Access chatbot, ‘I have a headache,’ Ochsner seeks to understand the acuity of the condition to know when a patient needs to see a neurologist. To drive the matching algorithms, Clearstep starts with a clinically trusted triage protocol (built in partnership with Dr. Barton Schmitt, co-author of the Schmitt-Thompson protocols) and follows with a series of conversational questions to present patients with clinically appropriate, timely and convenient Ochsner care options based on their specific symptoms and location.
“The use of Chatbots/LLM is a fantastic way to get patients to go through a decision tree and help them feel supported. When a patient types in ‘I have a headache’, the chatbot generates intelligent prompts to continue to triage, such as ‘Let’s get more information about your headache.’ ‘Does it seem like a migraine?’ ‘Have you had a longstanding headache for years?’ ‘Have you used medications without success?’ It is not just about a triaging protocol. It is about getting the information needed to match the patient with the right provider and care setting,” explains Dr. Jason Hill, Innovation Officer at Ochsner Health.
While Ochsner recognizes that some patients may know where to go for care, many patient conditions can be appropriately managed by low-acuity care services. An 2024 Clearstep analysis on user intent found that 73% of users had an incorrect intent of where to find care, the majority of which were de-escalated to a lower acuity. Ochsner’s data supports this finding. Out of 7,500 completed chatbot interactions, 77% benefitted from a low-acuity care modality (e.g. Virtual Urgent Care, Primary Care) for their symptoms.
“At Ochsner, like other health systems, we don’t just have neurologists, we have movement disorder specialists. We don’t just have ophthalmologists, we have neuro-ophthalmologists. These people are super- specialized. Anytime you put them with a patient that is not in their field, you are delaying care for someone with an urgent need for that specialist’s expertise – in a way, wasting that expert’s value,” explains Dr Hill. “As a large health system, it is our challenge to create a funnel which accounts for that level of complexity to the individual patient/provider interaction.”
The first step of creating the triage match is to set up the list of providers on the supply side. “We ask our super specialists to share common symptoms, complaints and situations. Then we try to figure out a way to get the patient to match those. We determine the questions that we need to ask to gather information that will enable us to make the right match,” says Dr. Hill.
“We work on identifying the right destination of care and sorting out whether a problem is acute or chronic. We do this using existing structures, as the patient moves through a protocol. As these decision-making tools become more sophisticated, we can then determine the provider type, and then, the sub-provider type,” Hill says. “At first, we are using decision trees, but the ultimate goal is to use AI to understand the patient and provider scope, as well as provide dynamic questions that allow us to establish the patient’s ultimate destination.”
“We need to train a model about what patients are asking us for each type of specialist -- and with that information we can create different models which have access to different aspects of these complex algorithms (e.g. payor coverage, specialist expertise). The AI will learn from our data to help sort the patient to the right match. Of course, the patient has the right to go wherever they wish, but the models can help to direct them to the most appropriate provider,” says Hill. “Once the patient matches, the specialist has access to that patient’s record to provide needed care. We can say to the specialist, ‘This is the right patient for you.’”
“The biggest value that the Clearstep Smart Access tool provides for Ochsner is getting the patient to the right place at the right time. So many patients end up in the ER for a simple rash. That is a waste of resources. Everyone wins when the patient ends up at the right level of care,” explains Ted Hudspeth, MD, Associate CMIO, Ochsner Health.
Of the users that complete a Clearstep conversation and receive a care recommendation, 56% engage with one of the three presented options that is determined to be the right level of care. This far exceeded Ochsner’s outset benchmark goal of 35%.
Clearstep regularly reviews user feedback to monitor and improve product performance of the core product. Ochsner also closely monitors the CSAT scores for the Ochsner instance to ensure that feature enhancements (e.g., displaying additional location services or appointment availability) enhance the user experience. Ochsner patients who have used this intelligent triaging chatbot have shared their positive experiences, noting that the chatbot was "easy to navigate" and offered "excellent service."
2. Supercharging PCPs with Specialist eConsults using Epic. 
Since a patient might not be able to see a particular specialist quickly, Ochsner is empowering the Primary Care Doctor to tee up patient questions to gather needed information from the specialist eConsult. “We are working with Epic to develop these templates designed to capture patient information to support specialist clinical responses and are feeding them into an LLM,” shares Dr. Hill.
“We started by capturing the ‘pearls’ or questions that each specialist needs the PCP to capture upfront and we built these pearls into each template,” Dr. Hudspeth explains. “This is valuable, since the PCP may not know all the questions to ask the patient for some conditions. Since this eConsult is asynchronous, it is essential to capture this information for the specialist to give the best response.”
The PCP fills in the template about the patient’s current health issue and receives the specialist’s protocol (e.g., do this, then this) response. If that does not work, the patient sets up a specialist appointment. The eConsult enables PCPs and patients to get answers quickly and reduces the number of patients needing the specialist referral.
“We have learned that this supercharged eConsult educates PCPs, who are really becoming triage experts. The next time a patient has a similar problem, the PCP knows what to do and is more empowered with back up information so they feel like they can do it,” Dr. Hill explains.
Ochsner has been building the specialist eConsult for their PCP network and has over 20 specialty areas covered. Dr. Hill explains, “There are certain specialties that are ripe for this workflow, like endocrinology, ID, and dermatology since they do not require as much of an in-person exam to render recommendations as some other specialties do. We started with these specialties, and as the project has grown, we have learned of others where the PCP can manage patients in place instead of sending them for a specialist appointment. The templates are being developed to help these departments with high numbers of eConsults to perform them easier.”
Ochsner is evaluating success factors including:
- Percentage of patients who needed to see a specialist (after the eConsult)
- Turnaround time for eConsult vs in- person appointment
- Care access for patients in regions without specialists
“We are doing over a thousand eConsults per month. Our PCPs feel they are delivering a higher level of care instead of sending the patient to wait for a specialist appointment, and getting a faster turnaround time on response. We request a 72-hour/3-day response for the eConsult, and we are seeing an average eConsult response of 1 ½ days across our specialty areas,” shares Dr. Hudspeth. “For the Ochsner system, 85% of patients have not needed an in-person visit within 90 days of eConsult and only 7% of eConsult requests converted into an in person and/or virtual appointment. eConsults help us free up capacity for our patients.”
Future AI- Driven Patient Care
Ochsner is analyzing the data from these AI tools to gain insights into the distribution of recommended care and patient preferences enabling them to understand service demand, evaluate system capacity, and dynamically promote the services that offer the best access for that patient. Ochsner is also envisioning how AI bots can help guide patients through the clinical maze, not only assisting with care navigation but also supporting patients through their care journey.
On the eConsult front, Dr. Hudspeth explains: “We are excited by the future of AI and our work with Epic. AI is designed to get answers, but it does not know the questions. We have the questions that specialists want answered.”
Ochsner views the responsible use of AI tools as critical differentiators and catalysts to help drive better patient care, and that starts with access and communication.
“These tools are evolving at a rapid pace, but without collaboration with patients and clinicians, and thoughtful workflows which take advantage of our network of skilled providers, they are useless. AI technology has the potential to transform care for the better. We must consider how these technologies might impact our patients and providers and carefully decide how to use them to evolve our care model. With each iterative step, these tools are guided by our clinical and connected health teams to make sure they are providing value,” Dr. Hill concludes.
 Permalink
Permalink  Care Journey,
Care Journey,  Triaging,
Triaging,  eConsult in
eConsult in  AI,
AI,  AI Healthcare,
AI Healthcare,  AI consumer engagement,
AI consumer engagement,  Care Coordination,
Care Coordination,  Care access,
Care access,  Care collaboration,
Care collaboration,  Chatbot,
Chatbot,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision support,
Decision support,  Patient Centered Care Design,
Patient Centered Care Design,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Virtual Health Assistant,
Virtual Health Assistant,  digital health
digital health