During the Voice.Health Summit in Boston last week, innovators gathered to explore opportunities, discuss issues and to experience different voice technology use cases.
 BCH John Brownstein shares voice health use casesJohn Brownstein, Chief Innovation Officer at Boston Children’s Hospital is excited about the opportunity for healthcare to lead other verticals with this empowering technology which many of us use every day – Alexa tell me… Siri what is… ?
BCH John Brownstein shares voice health use casesJohn Brownstein, Chief Innovation Officer at Boston Children’s Hospital is excited about the opportunity for healthcare to lead other verticals with this empowering technology which many of us use every day – Alexa tell me… Siri what is… ?
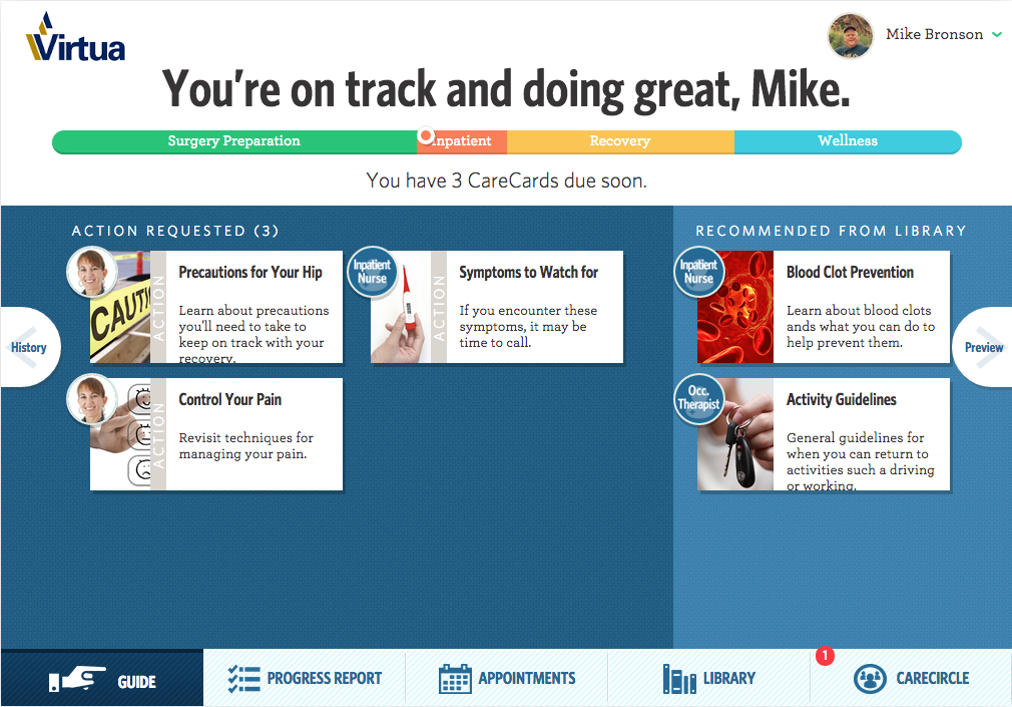
Since the year 2000, the health technology industry has evolved from websites (e.g. patient portals) to mobile applications (mhealth) and now to voice and conversational assistants. There are many use cases which help patients and providers in different settings.
- In hospital, the doctor asks to see the patient’s latest lab results.
- Following a hospital discharge, the patient interacts with his virtual robot to record side effects from his new medications.
- Preparing for an outpatient visit, a patient verbally responds to the pre-visit questions to share with her doctor.
- Days after a remote monitoring visit, a patient asks additional questions to help her manage her asthma.
Although voice health technology is in the early adoption stage, health innovators are convinced that these virtual voice assistants can address real problems -- the shortage of healthcare professionals, clinician burn out, inefficiencies in patient care, lack of patient engagement and the inability to personally support patients along their health journey outside of the hospital. Nuance’s Peter Durlach stresses the importance of using these technologies to free up the clinicians to take care of patients.
Voice has many unique benefits for healthcare. Dr. Rupal Patel, CEO VocalID describes the convenience (e.g. hands free), the capability to capture information and insights about the user (e.g. gender, size, bio- markers) and ability to generate trust through continuous listening and personalized responses. Other benefits include the ability to capture context (e.g. surroundings, urgency and intent) and empower the user (e.g. patient feels a sense of control). Amazon’s Emily Roberts, Sr. Marketing Manager adds the value of capturing “moments of the day” by incorporating voice into other devices (e.g. smart home/refrigerator, car).
Voice Health in Action
During the Voice.Health Summit, we saw what “voice-first” can deliver in five different care setting exhibits. Here are some interesting examples of use cases to bring value to patients and/or the care team.
1. Hospital/Patient. With the Joint Commission’s focus on “accurate screening and assessment of pain”, Dr. Samir Tulebaev, Geriatrician and the Center of Nursing Excellence at Brigham and Women’s Hospital are working with Orbita’s CEO Nate Treloar on the development of a post- operative pain management voice assistant. The patient tells her bedside teddy bear Briggie (which has a built in microphone) that she is in pain, describes where the pain is and indicates if the pain is intolerable. Her nurse immediately receives a secure text message to respond.
2. Hospital/Clinical. Cedars-Sinai uses Sopris Assistant to record, summarize, approve and place the patient care note into the EHR. The AI summons the listening technology, drives the summary and produces the intelligent note for physicians. Cedars-Sinai helped Sopris Health create an experience and workflow catered to hospitalist.
3. Senior Living & Home Health. Caregivers can engage an aging patient with the AI powered LifePod virtual assistant which serves as a personalized companion, delivers reminders, and monitors daily activities. LifePod’s CEO Stuart Patterson emphasized the importance of “proactive voice” which shares and captures essential information without relying on the person to ask (i.e. reactive voice).
4. Consumer Home. Anne Weiler, CEO Wellpepper, the winner of the Alexa Diabetes Challenge, engages a patient who is recently diagnosed with type 2 Diabetes. She uses her voice to weigh herself, scan her feet for ulcers and track her care plan tasks. This voice assistant gives the patient an opportunity to proactively engage whenever she wants.
5. Vocal Biomarker Lab. Sonde Health is interested in capturing and using a patient’s voice samples as health measures for different physical (e.g. sinus congestion) and mental health conditions (e.g. depression, suicide risk).
Lessons from Voice Health Innovators
As with any new technology, there is a lot to learn from the pioneers.
Real Problem Definition: Sara Holoubek, CEO Luminary Labs emphasized the importance of deciding who (e.g. newly diagnosed) and what (e.g. help with self-management) as a first step to focus the development planning process.
Patient/User Input: Deloitte's Debbie Hays, Specialist Executive discussed the patient journey research for the DeloitteASSIST voice solution which revealed the “challenges and delays” that needed to be addressed while the patient is in the hospital room.
Patient/User Feedback: Karin Beckstrom, Sr. Product Manager ERT Innovation Lab (formally PHT) described using voice to capture patient reported outcomes (PROs) on a daily basis. We ask-- how engaging was it? Are you willing to answer questions on a daily basis? How difficult was the skill? Did Alexa understand you?
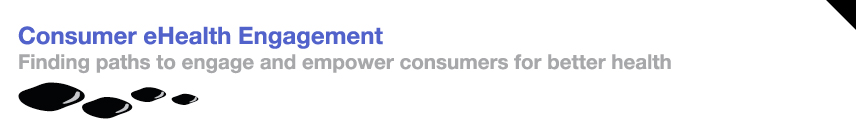
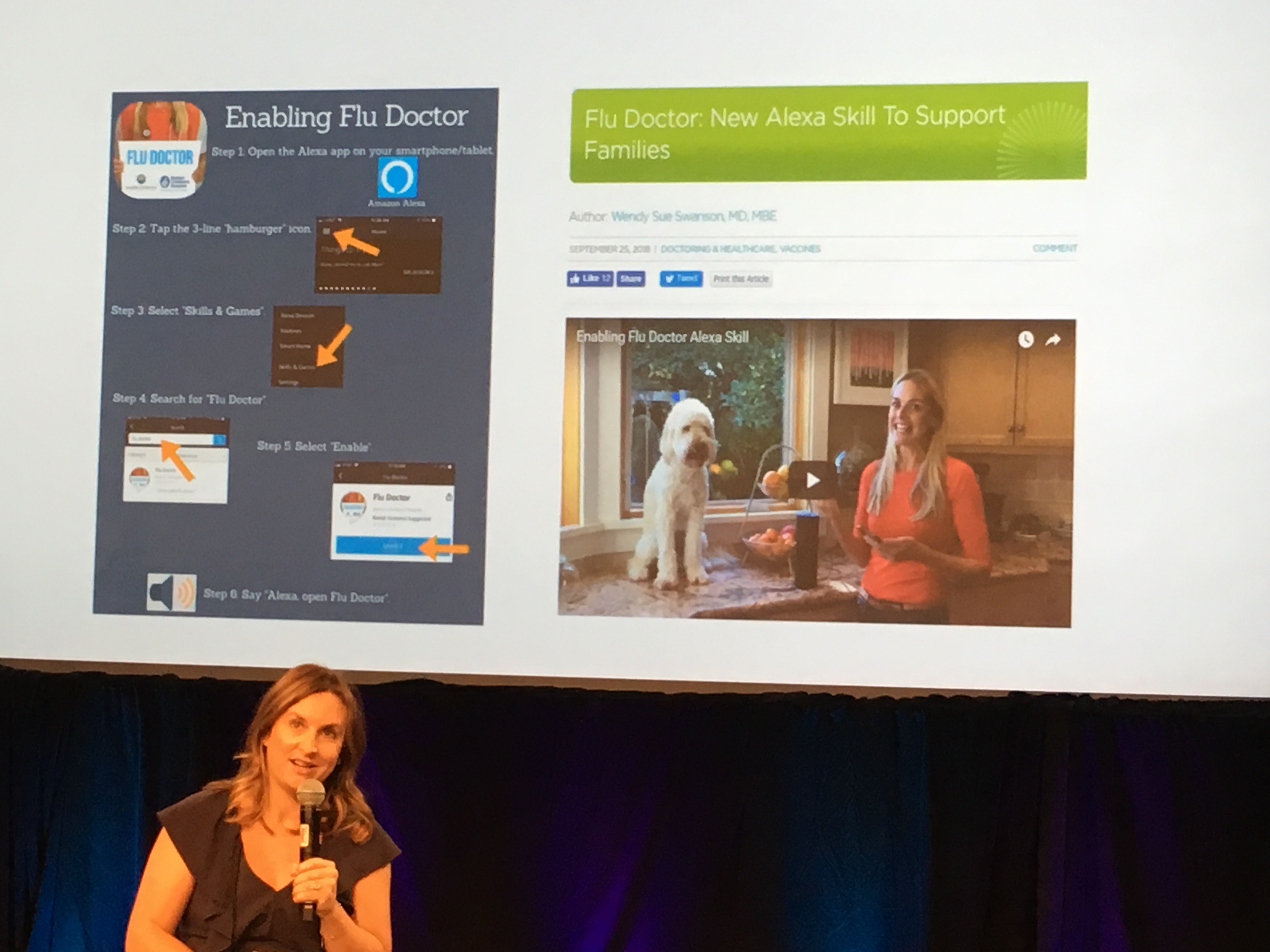 "Flu Doctor" from Seattle Children's Hospital Stacey UlaciaPersonalization: Stacey Ulacia, Sr. Communications Specialist at Seattle Children’s Hospital in partnership with Boston Children’s Hospital, developed the “Flu Doctor” voice skill. This brings more value since it is customized based on the zip code provided by the patient.
"Flu Doctor" from Seattle Children's Hospital Stacey UlaciaPersonalization: Stacey Ulacia, Sr. Communications Specialist at Seattle Children’s Hospital in partnership with Boston Children’s Hospital, developed the “Flu Doctor” voice skill. This brings more value since it is customized based on the zip code provided by the patient.
Opportunities for Voice to Solve Healthcare Problems
There are many use cases for voice technology to help drive the triple aim.
UPMC’s Dr. Shivdev Rao believes it would be valuable to use voice to help triage a care situation, and capture information from the patient pre or post exam.
Boston Children’s Hospital Dr. Docktor shared Pediatrics Voice Hackathon examples including one which uses voice to help a patient prepare for his procedure at home with instructions and images that are tailored to his specific health issues (e.g. food problems).
Cedars-Sinai Medical Center in Los Angeles is collaborating with Sumeet Bhalitia, Founder & CEO Avia to bring voice into the hospital room, giving the patient control over their experience and the ability to get assistance as needed (e.g. bathroom help) with the goal of increased patient satisfaction.
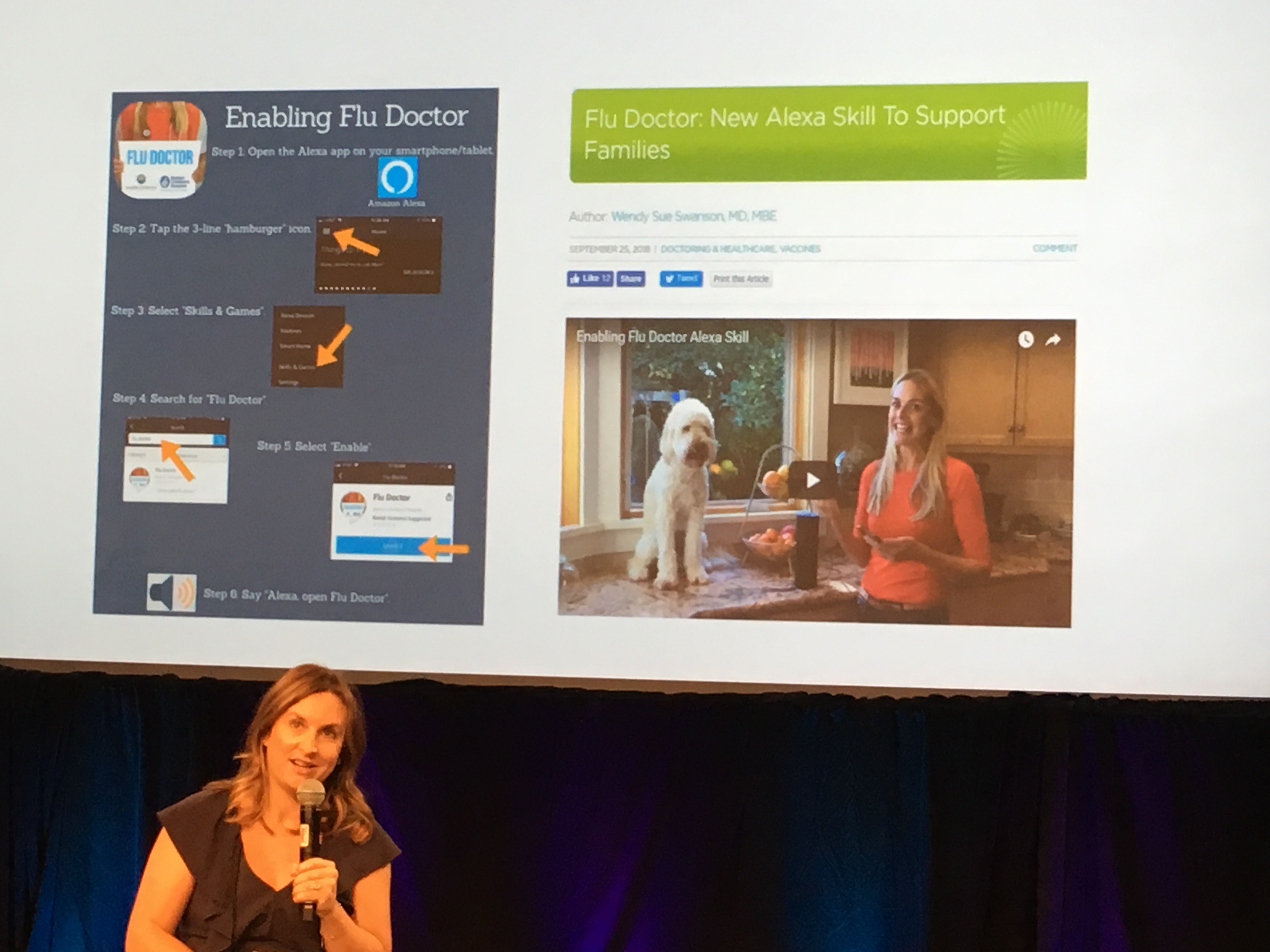
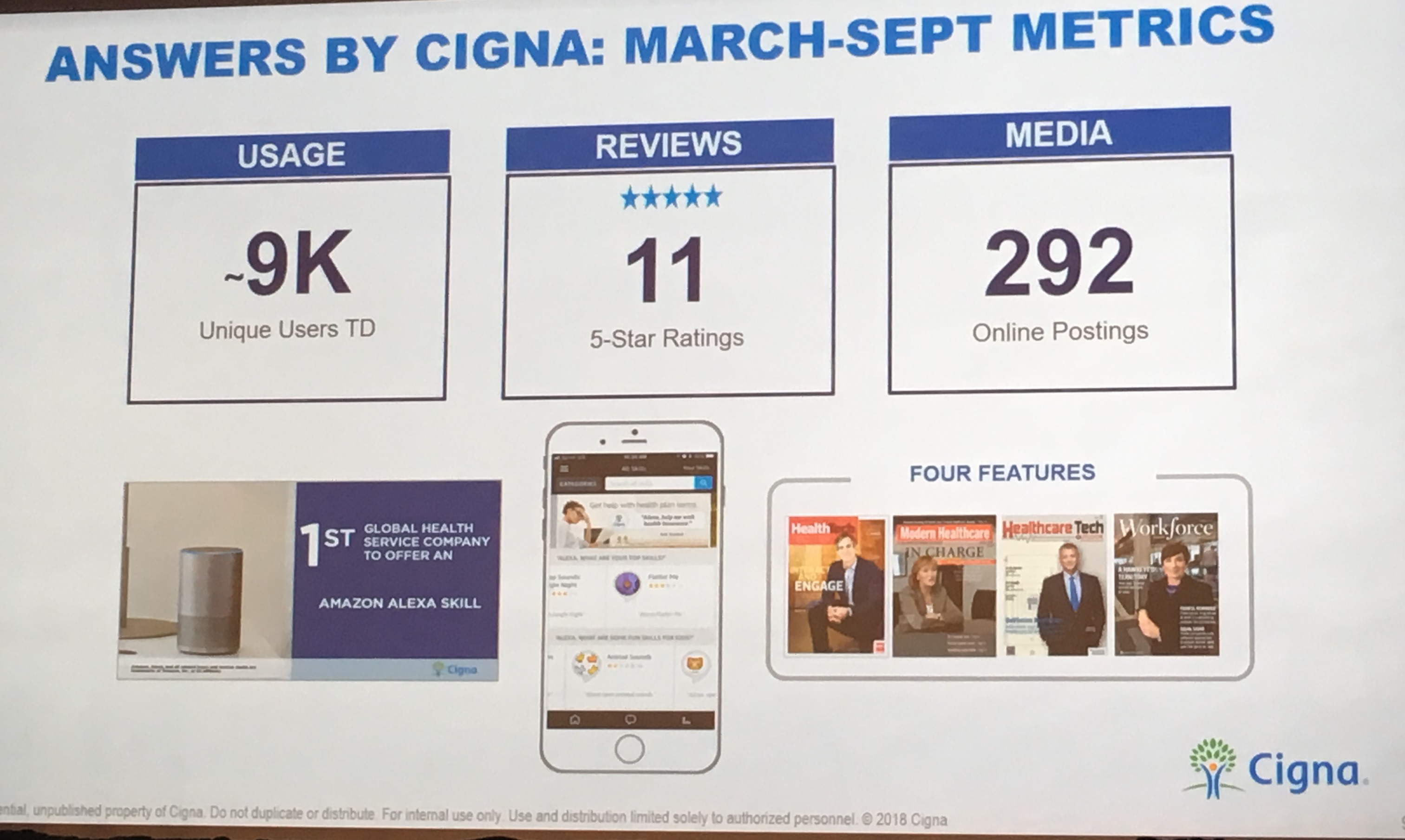 Recent metrics for Answers by CignaCigna’s Laura Schuntermann, Global Head of Digital Strategy & Partnerships is excited by the growth of voice search. Gartner predicts by 2020, 30% of searches will be voice activated. Laura shared results from the voice solution Answers by Cigna which helps members get the information they need to make better health care decisions.
Recent metrics for Answers by CignaCigna’s Laura Schuntermann, Global Head of Digital Strategy & Partnerships is excited by the growth of voice search. Gartner predicts by 2020, 30% of searches will be voice activated. Laura shared results from the voice solution Answers by Cigna which helps members get the information they need to make better health care decisions.
Novartis’s Robert Stevens, Executive Director of Digital Strategy & Medical Innovation described voice health use cases that help clinicians determine the diagnosis/clinical decision support, check guidelines, send RXs to pharmacy and order follow up patient education.
Future Voice Health Considerations
Although there is excitement around voice health, innovators are working to remove speed bumps to accelerate adoption:
Addressing Privacy/Security. Several organizations are anxiously awaiting for HIPAA compliant voice devices. There is also a concern that the device is always listening, even without the “wake” word.
Educating Patients about Voice. A few presenters admitted that patients do not know what they can ask. This means that either they are not using all of the voice capabilities or the patient has an unexpected experience -- Alexa says …. Hmm I do not know that one.
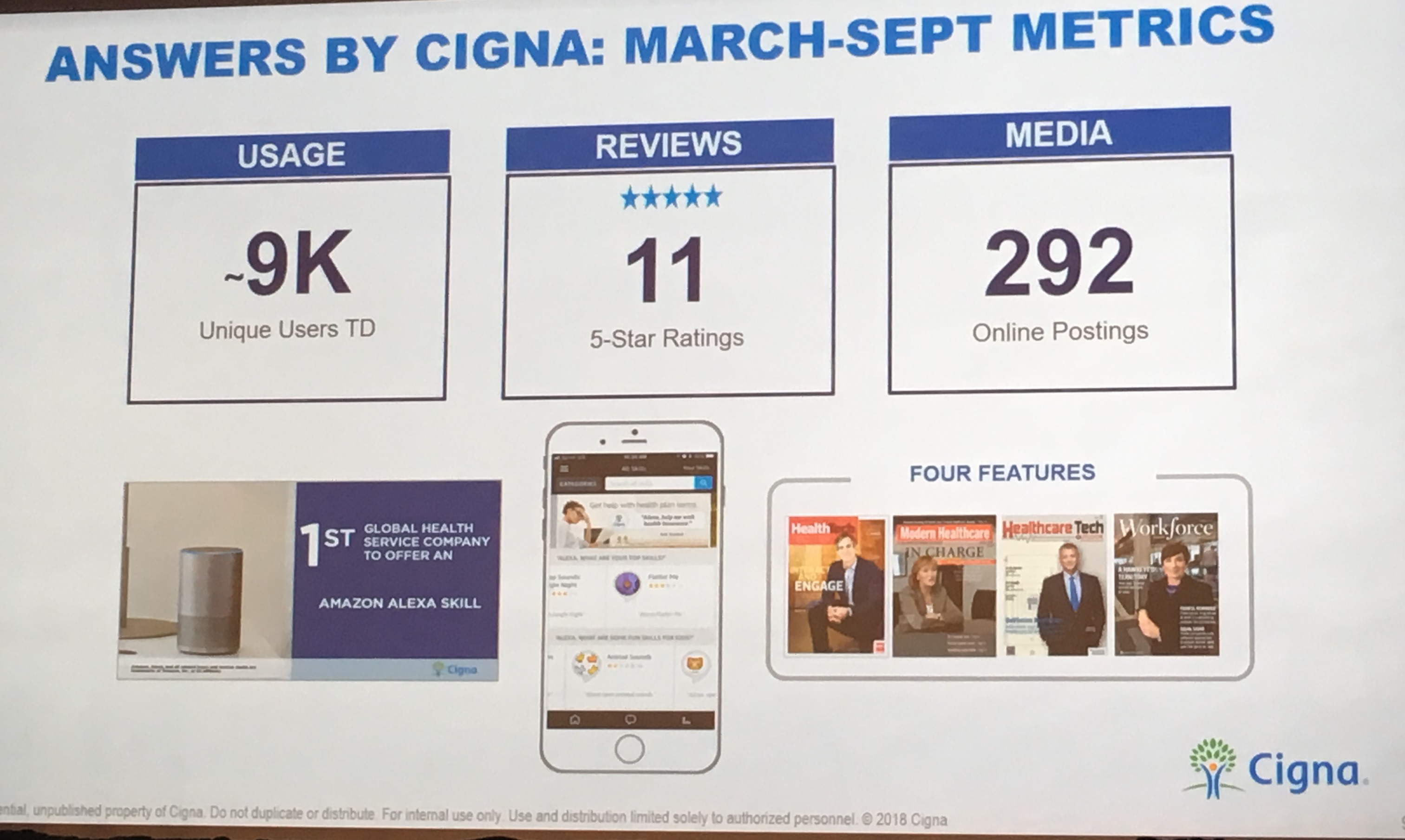
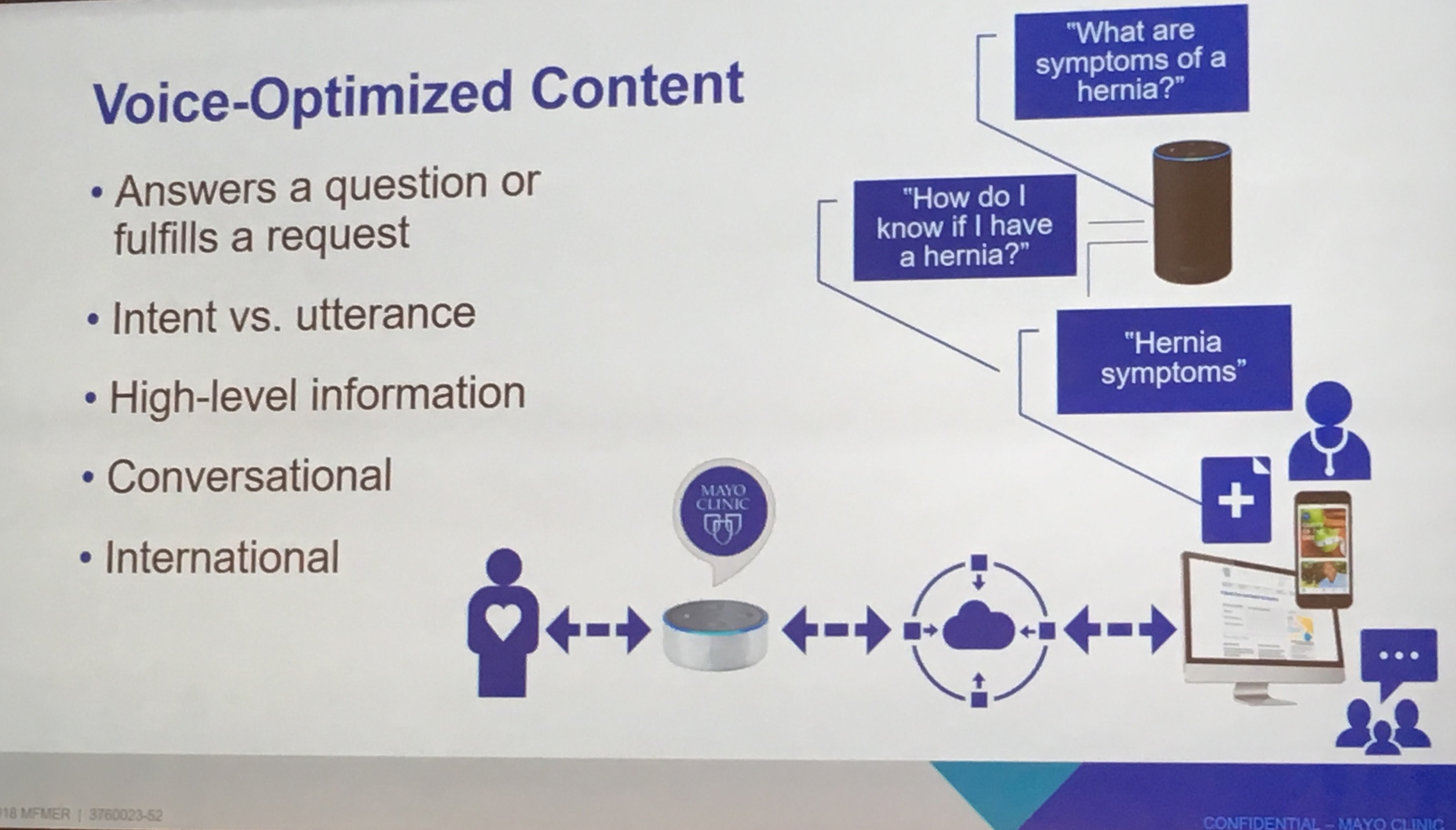 Mayo Clinic's Optimizing Voice Content Creating complete Patient Experiences. Mayo Clinic’s Jennifer Warner, Sr Editor Global Business Solutions explains that voice is additive and does not replace other consumer engagement methods. Therefore, it is important to provide an “omni-channel” experience to engage and support the patient through every touch point.
Mayo Clinic's Optimizing Voice Content Creating complete Patient Experiences. Mayo Clinic’s Jennifer Warner, Sr Editor Global Business Solutions explains that voice is additive and does not replace other consumer engagement methods. Therefore, it is important to provide an “omni-channel” experience to engage and support the patient through every touch point.
Collaborating on Care Design. Maia Ottenstein, Digital Experience Design at Thomas Jefferson University Hospital (DICE/design group within the hospital) is working on the “smart patient concierge” which empowers the patient to access assistance and resources on demand.
It will take a community of patient and clinical stakeholders to define, design and deliver voice technologies that bring real value to the users. It is encouraging to see that these stakeholders are coming together in hospitals, accelerators and innovation hubs to bring these voice technologies to life.
 Permalink
Permalink  care collaboration,
care collaboration,  chronic care management,
chronic care management,  patient generated health data in
patient generated health data in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Decision support,
Decision support,  Mobile Health,
Mobile Health,  Patient Centered Care Design,
Patient Centered Care Design,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Patient Journey,
Patient Journey,  Patient Portal,
Patient Portal,  Population Health,
Population Health,  Population health management,
Population health management,  TeleMedicine,
TeleMedicine,  digital health,
digital health,  online coaching,
online coaching,  patient health education
patient health education