Entries in personalization for health and wellness (23)
Boston Children’s, Brigham and Women’s & Northwell Health leverage virtual assistants for a better patient care experience
 September 27, 2019
September 27, 2019  During the World Congress Patient Experience & Engagement Summit in Boston, I led a panel with these innovative health systems, discussing how they are using virtual health assistants (e.g. AI Chatbots, Voice) to increase efficiency in care delivery and enhance the patient experience.
During the World Congress Patient Experience & Engagement Summit in Boston, I led a panel with these innovative health systems, discussing how they are using virtual health assistants (e.g. AI Chatbots, Voice) to increase efficiency in care delivery and enhance the patient experience.
Virtual Assistants in Healthcare
Consumers are demanding convenience and want to interact with companies any time anywhere. Companies across different industries such as retail, travel and financial services are responding with virtual assistant tools, enabling consumers to get answers and transact 24x7.
Within healthcare, innovation driven organizations are exploring how to empower patients with virtual health agents to access relevant care information (e.g. learn about how to prepare for a procedure, determine when to call the doctor following surgery), get tasks done (e.g. schedule and participate in a virtual visit) and get guidance on a care plan (e.g. reminders to refill medication, follow up doctor’s appointments).
The strong interest in AI driven virtual health assistants aligns with Accenture’s Digital Health Tech Vision 2019 trend #5 “MYMARKETS: Meeting customer’s needs at the speed of now”. The Accenture report explains “digital expectations have now evolved and a new opportunity to deliver better experiences is on the table: capturing moments. Technology has created a world of intensely customized and on-demand experiences, so healthcare organizations must reinvent themselves to find and capture those opportunities as they come”.
Value of Virtual Health Assistants
When you think about the gaps in healthcare efficiency today, you can envision how virtual health assistants can support patients and the care team.
There are many valuable use cases for Virtual Health Assistants to help patients prepare and manage their care, with reminders, education (e.g. health condition, procedure) and the capability to escalate to a care provider as needed.
On the clinical side, the care team can capture, monitor and communicate with patients. Instead of making outbound calls trying to reach patients, staff can see which patients are in pain, have questions/concerns or are in need of immediate care.
Panelist Virtual Health Assistant Use Cases
When presenting their use cases for Virtual Health Assistants, panelists shared their specific business goals such as decreasing readmissions/ED visits and costs, increasing service utilization, improving care plan compliance and enhancing the patient experience. All panelists view these virtual health assistants as an “extension” of their care delivery.
 Boston Children’s Hospital (BCH): In 2018, BCH teamed up with Seattle Children’s on an Alexa skill, Flu Doctor, providing parents with answers to questions about the flu which are “personalized, science-backed data and recommendations”. Panelist Devin Nadar, Senior Partnerships Manager, Innovation and Digital Health Accelerator discussed a more recent Alexa skill -“My Children’s Enhanced Recovery After Surgery (ERAS)”, which is part of the program for all cardiac patients undergoing specific surgeries at BCH. Built on the Amazon platform, this skill to desgned to capture information from the parent about how the child is doing after the surgery and indicate if there is a follow up appointment scheduled. “We know that parents really don’t want to come back to the hospital after surgery”, Devin adds. After accessing “My Childrens” through the Amazon Alexa Store, the parent begins to “check in” the day after the patient is discharged and receives pertinent information for that day.” Before this tool, it was “like a black box” about what happens while the patient is recovering. Now BCH can focus clinical resources on patients with priority needs.
Boston Children’s Hospital (BCH): In 2018, BCH teamed up with Seattle Children’s on an Alexa skill, Flu Doctor, providing parents with answers to questions about the flu which are “personalized, science-backed data and recommendations”. Panelist Devin Nadar, Senior Partnerships Manager, Innovation and Digital Health Accelerator discussed a more recent Alexa skill -“My Children’s Enhanced Recovery After Surgery (ERAS)”, which is part of the program for all cardiac patients undergoing specific surgeries at BCH. Built on the Amazon platform, this skill to desgned to capture information from the parent about how the child is doing after the surgery and indicate if there is a follow up appointment scheduled. “We know that parents really don’t want to come back to the hospital after surgery”, Devin adds. After accessing “My Childrens” through the Amazon Alexa Store, the parent begins to “check in” the day after the patient is discharged and receives pertinent information for that day.” Before this tool, it was “like a black box” about what happens while the patient is recovering. Now BCH can focus clinical resources on patients with priority needs.
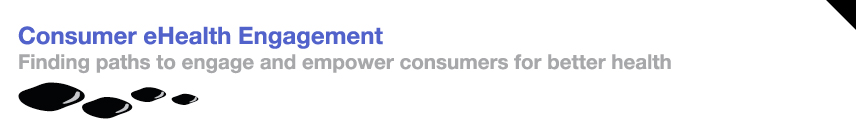
 Dana-Farber/Brigham and Women's Cancer: “Earlier this year we developed and are planning to launch an Orbita powered health assistant to support prostate cancer patients who are on a “lifelong journey” with ongoing PSA testing” shares Rich Boyajian, NP Program Director, Virtual PSA Monitoring, Radiation Oncology. This chatbot will send a link to the patient to engage via text and/or voice on their phone. It is designed to “onboard” him into the program, present the closest lab, deliver good PSA test results and enable him to request contact with a care team member. “Patients can select the modality for this follow up contact by email, a call or even a virtual visit”, explains Rich. “It was easy for me to write the virtual health assistant script (i.e. questions and answers) to engage with the patient since I do this all the time. We selected the Orbita platform because we can put this content in one time and it be accessed by the patient through their preferred modality”.
Dana-Farber/Brigham and Women's Cancer: “Earlier this year we developed and are planning to launch an Orbita powered health assistant to support prostate cancer patients who are on a “lifelong journey” with ongoing PSA testing” shares Rich Boyajian, NP Program Director, Virtual PSA Monitoring, Radiation Oncology. This chatbot will send a link to the patient to engage via text and/or voice on their phone. It is designed to “onboard” him into the program, present the closest lab, deliver good PSA test results and enable him to request contact with a care team member. “Patients can select the modality for this follow up contact by email, a call or even a virtual visit”, explains Rich. “It was easy for me to write the virtual health assistant script (i.e. questions and answers) to engage with the patient since I do this all the time. We selected the Orbita platform because we can put this content in one time and it be accessed by the patient through their preferred modality”.
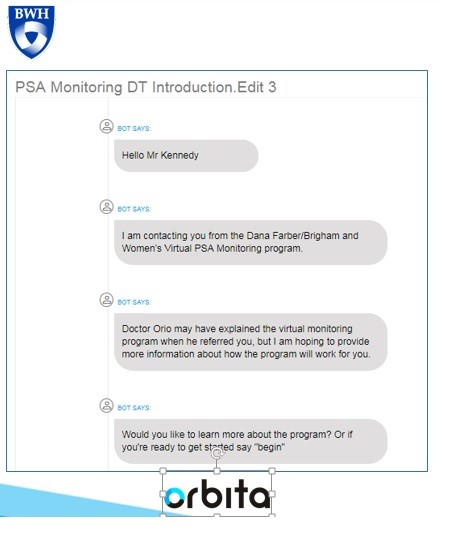
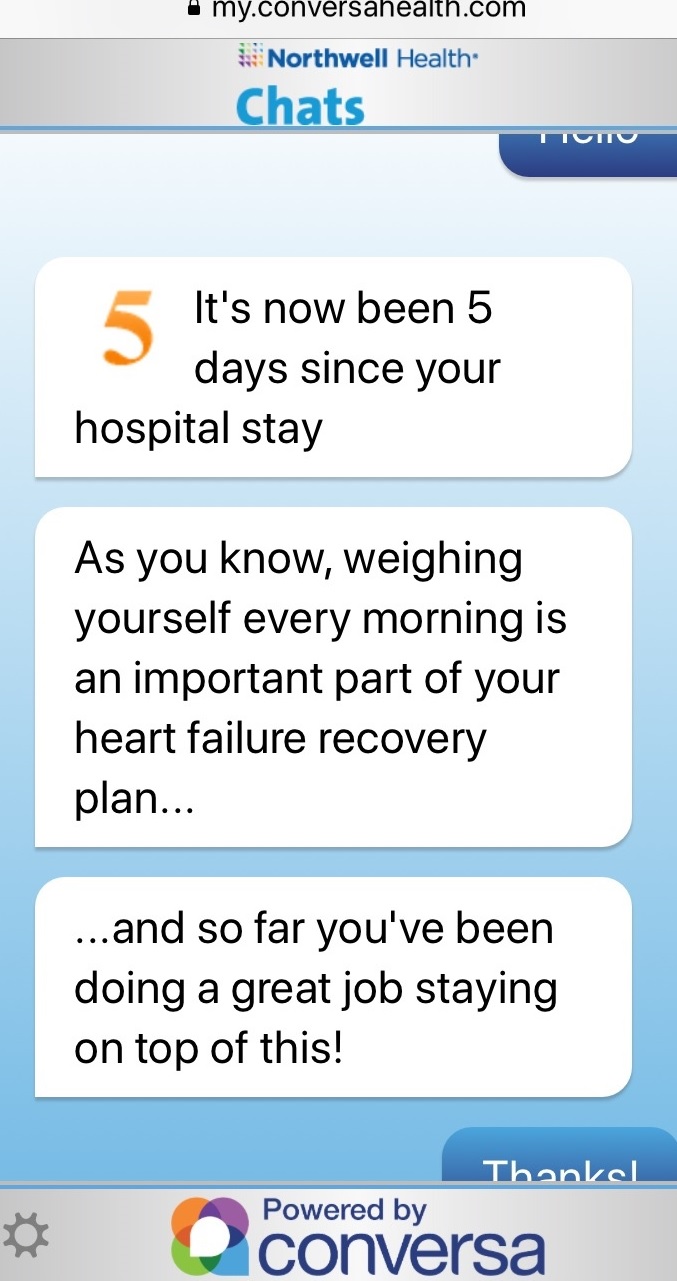
 Northwell Health: In 2018, Northwell launched Health Chats, an AI text chatbot powered by Conversa Health, which empowers patients to stay connected to their care navigator through recovery. This gives the staff visibility into what is really happening when the patient leaves the hospital. “We selected Conversa Health because it is easy for the patient who doesn’t need to download an app. Instead the patient receives a chat notification through an email or SMS text message and simply clicks on the link to start the chat through their mobile phone”, explains Hallie Bleau, ACNP-BC, AVP Transitional Care Management, Health Solutions. The Health Chat engages the patient post discharge to “self -assess and manage symptoms”. Since Northwell Health integrated the Health Chat into their care management system, the information that the patient types in (problems, pain level) is feed into an algorithm to flag the patient on the nurse’s dashboard for an immediate contact. The patient can connect with a nurse through the Health Chat application at any time.
Northwell Health: In 2018, Northwell launched Health Chats, an AI text chatbot powered by Conversa Health, which empowers patients to stay connected to their care navigator through recovery. This gives the staff visibility into what is really happening when the patient leaves the hospital. “We selected Conversa Health because it is easy for the patient who doesn’t need to download an app. Instead the patient receives a chat notification through an email or SMS text message and simply clicks on the link to start the chat through their mobile phone”, explains Hallie Bleau, ACNP-BC, AVP Transitional Care Management, Health Solutions. The Health Chat engages the patient post discharge to “self -assess and manage symptoms”. Since Northwell Health integrated the Health Chat into their care management system, the information that the patient types in (problems, pain level) is feed into an algorithm to flag the patient on the nurse’s dashboard for an immediate contact. The patient can connect with a nurse through the Health Chat application at any time.
Panelist Insights on Virtual Health Assistants
Many lessons learned were shared by the panelists including considerations for both patient and staff engagement. One common theme was that the planning for these Virtual Health Assistants takes time. “We needed 6-8 months to get staff buy- in and patient consent”, admits Hallie.
Patient Considerations:
Determine fit with the patient’s current technology. “With our 65+ Medicare population at Northwell Health, we realized that one big barrier was some patients still have a flip phone which will not work with our chatbot”, Hallie explains.
Understand patient expectations. “In our Alexa skill, we ask if the caregiver would like the doctor/nurse to call. We know there are differences in how long the call back will take so we need to set the proper expectations for when they can expect a return call ”, shares Devin.
All panelists expressed an interest in learning from patients about their experiences. “We built into the Alexa skill ‘did that answer your question’ so that we can capture their feedback and make changes to our script”, Devin explains.
Patients have shared insightful comments about their virtual health assistant interactions. “Our patients at Northwell Health feel that someone is always thinking about them. In a 30 day period, we are able to increase the number of touches by 5-6 contacts”. Hallie went on to say “we thought that caregivers would be more interested in seeing these digital conversations with mom. We learned some didn’t because ‘she doesn’t live with me’. Several seniors do not want to ‘bother their daughter with this information’. We have also learned that patients who are hard of hearing really like to use the chatbot because it is easier to communicate with the care team”.
Staff Considerations:
During the planning stages, panelists feel it is important to educate their staff. They need to feel comfortable with this new digital interaction, understand how to describe it to patients and have a clear picture how this will impact their workflow. Specific considerations include:
Extensive staff education. “We were surprised at the amount of time/education required with our staff. They needed to understand why and what does it mean for them”, admits Hallie.
Devin adds “we train with our staff, demonstrate the app and provide a cheat sheet for reference, which tells about them about our Alexa skill, how to open it, start it, stop it, what you can ask and what it is used for”.
Stage the implementation. “We have limited the roll out of the voice app to 5-10 per week because we did not want to overwhelm our staff at BCH”, explains Devin.
Success Measures & Future Virtual Health Assistants
Later in the year, panelists will be evaluating their program from an experience (patient, staff), operational efficiency and clinical perspective.
“At BCH, we want to see if parents are completing the questions and determining where they drop off so that we can build a better experience”, describes Devin.
“Our virtual health assistant is replacing the manual labor from looking up the nearest lab to calling cancer patients about positive test results”, shares Rich. “As an extension of our care, we expect to decrease the number of follow up in person visits which will free us up to care for more patients”.
“Our staff is seeing the fruits of labor… ‘we don’t have to call him’, ‘we can quickly get to the root of the problem”, adds Hallie.
Panelists expressed the need in the future to capture and place pertinent information from the digital health interaction into the patient’s electronic medical record.
Future Plans:
Refine conversation based on role. “At Northwell Health, we are talking about tweaking the conversation for the caregiver”, explains Hallie.
Expand languages. “We currently offer our chatbot in English and Spanish but will add other languages”, Hallie shares.
Add new capabilities. “We plan to add more symptoms to our health assistant to provide more information for our PSA monitoring”, explains Rich.
Extend the Experience. “We are working on expanding the digital conversation from 30 to 90 days so that we have more insight into their receovery”, mentions Hallie.
Connect into Virtual Care. “At BCH, we are thinking about triggering a virtual visit when the parent indicates that she needs to speak with someone”, shares Devin.
Northwell Health is planning to continuously launch Health Chats across their organization given their strategic investment in ConversaHealth. “We have already launched Health Chats to patients with head and neck cancer and are getting ready to roll out them out in our cardiac surgery department” Hallie concludes.
Oncology Patients experience a personalized journey with interventions and education for better care
 January 15, 2019
January 15, 2019  The National Cancer Institute reports 2017 U.S. cancer care expenditures were $147+ billion, with anticipated increases from our aging population.
The National Cancer Institute reports 2017 U.S. cancer care expenditures were $147+ billion, with anticipated increases from our aging population.
According to Deloitte’s report in Evidence Based Oncology ( The American Journal of Managed Care publication), many organizations are exploring ways to control costs and enhance care quality for oncology patients (e.g. Patient Centered Medical Homes, CMS’ Oncology Care Model).
With many different types of cancer and treatment options, each patient embarks on a personal care journey.
Oncology patients often experience a long journey. Although some steps entail engaging with care staff at a hospital or clinic, most of the time patients are challenged with managing their disease on a daily basis away from the health system.
Healthcare organizations need to closely monitor oncology patients to determine when care and support is required. To be proactive and stay aligned with patient needs, health systems must collect patient information (e.g. Patient Reported Outcomes/PROMs, Patient reported experiences/PREMs). This patient information can guide the care team to intervene, reducing hospitalizations and costs.
Northwestern Medicine’s Oncology Program
“We wanted to take a holistic approach with our oncology patients; mind, body and spirit”, explains Dr. Martha L. Twaddle MD FACP FAAHPM HMDC, Medical Director - Palliative Medicine & Supportive Care, Northwestern Medicine, Lake Forest North Region. “We wanted to help our patients navigate their oncology journey, figure out their new normal and participate in their care”.
“A few years ago, we successfully used a patient engagement care tool with our palliative patients. Our palliative team is embedded within Oncology. Eighteen months ago, we introduced this telehealth type of application to our oncology patients. We felt it would be valuable to extend TapCloud to our general oncology patients because we had seen such a positive response using it for those with high symptom burden and advance disease. We believe many patients and caregivers will benefit from having this tool available to use”.
Patient Experience
How does TapCloud support the oncology patient? What is the patient experience?
 Last month, Robert (not his real name), a 77 year old patient was diagnosed with prostate cancer. Dr. Twaddle and her staff worked closely with Robert through the onboarding process to provide an overview, demonstrate how to use TapCloud, help him download the TapCloud app onto his phone and iPad and discuss what symptoms they will manage to personalize the app for his specific condition.
Last month, Robert (not his real name), a 77 year old patient was diagnosed with prostate cancer. Dr. Twaddle and her staff worked closely with Robert through the onboarding process to provide an overview, demonstrate how to use TapCloud, help him download the TapCloud app onto his phone and iPad and discuss what symptoms they will manage to personalize the app for his specific condition.
The Nurse Coordinator explained “Robert, with this tool (TapCloud), we can think about you when you are not in front of us, get a sense of how you are doing and that we are on the same page”. Robert was relieved to get a message from his Nurse Coordinator confirming that she can see Robert listed on the dashboard to keep a close eye on him.
Most of Dr. Twaddle’s seventy active patients using the TapCloud App are in their 60s and 70s, with a few in their 80s and 90s.
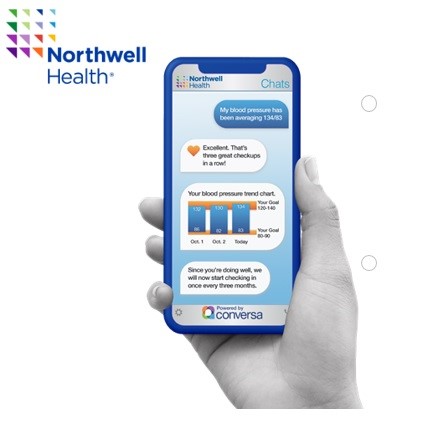
Through the TapCloud app Care Plan, patients like Robert are asked a set of questions. How are you feeling today compared with yesterday? Which of these meds are you taking? Which symptoms are you experiencing today? Symptoms that were selected the prior day are displayed bold. Patients can add symptom(s) which typically takes less than a minute to provide this critical information.
Symptom tracking is made easy by using a word cloud. Each day, the patient sees a personalized word cloud containing symptoms. This personalized symptom cloud incorporates his condition and medications and his list is continuously enhanced from machine learning. TapCloud’s predictive symptoms cover 100+ conditions and 14,000+ side effects. The patient simply touches those symptoms he is noticing. Additionally, he views personalized education based on his journey stage (e.g. tips for managing chemo side effects) and what he is experiencing. He can also upload this biometric information (e.g. vitals, etc.).
How has Northwestern Medicine used the TapCloud tool to deliver better care to Oncology Patients?
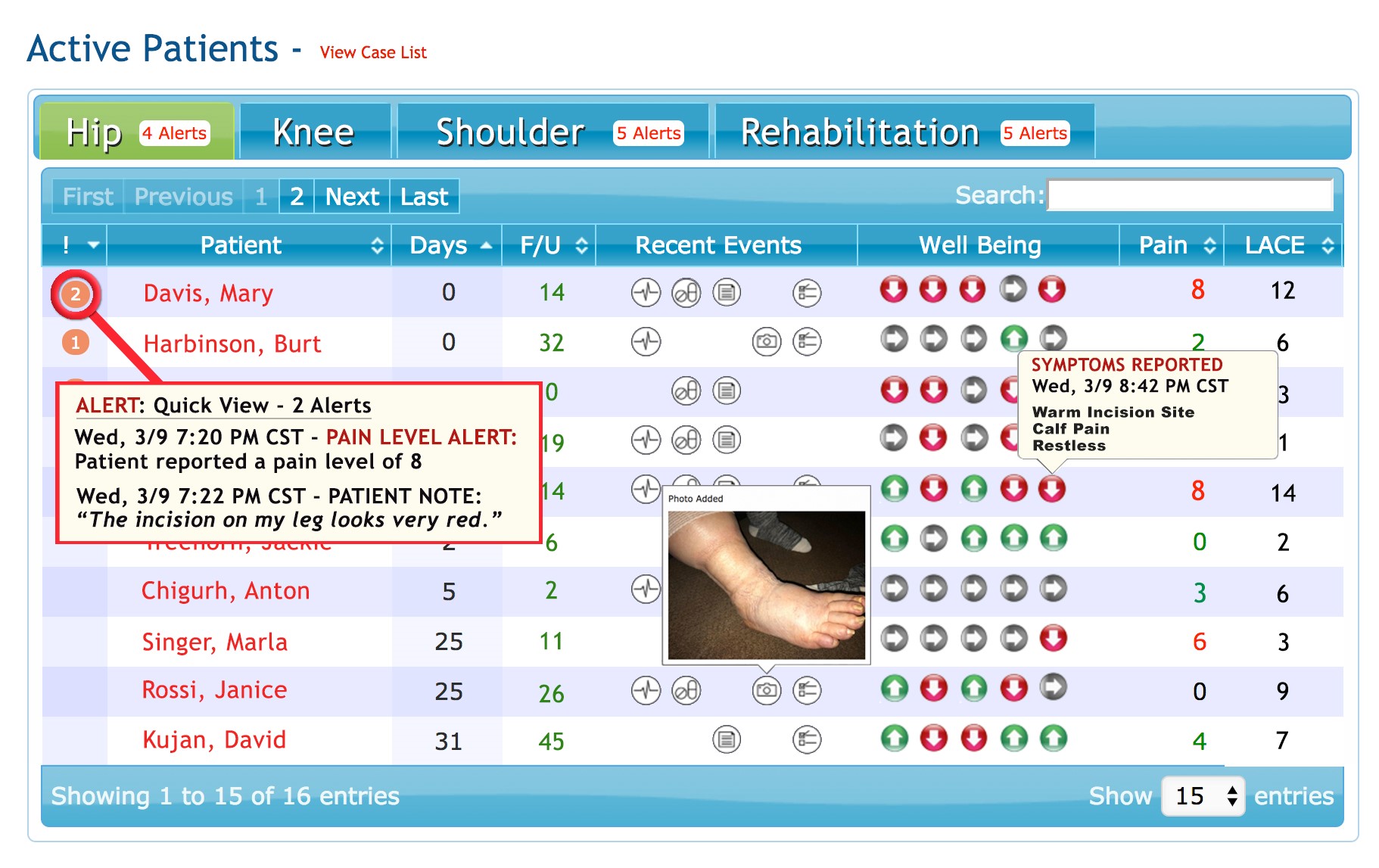 Dashboard displays demo data only
Dashboard displays demo data only
- Prioritize Patient Outreach. The TapCloud platform analyzes all the patient clinical and self- reported data in real time. Using advanced algorithms, patients with a clinical need are identified and alerts are sent to the care team. Patients are prioritized based on alerts, severity and risk. Nurses use the TapCloud Triage Dashboard to efficiently track, monitor and respond to patients requiring an intervention. Nurses can drill down on a specific patient to see how many days since check in, recent events (e.g. vitals, medication usage), pain and anxiety levels.
- Intervene on specific symptoms: Instead of “fishing” for information about how a patient is feeling or having the patient end up in the ER, Nurse Terri can call the patient and say “I've noticed that you've had increased pain the past 2 days…”. TapCloud can also be set up to send alerts for symptoms associated with a patient’s treatment. Patients can send a picture within the TapCloud app with a secure message about their concern.
- In the Patient’s Words: “We had one patient who didn’t feel pain but entered ‘yuk’. He selected that to communicate in his words what he was feeling. One of the features that I really like is journaling. A patient may share that today he is ‘discouraged by his illness’. Although he does not expect us to respond, it gives us insight into how he is doing and the support that he may need from us”, shares Dr. Twaddle.
- Stay Connected with patients who do not come in regularly: When patients are going through infusion treatment, Dr. Twaddle explained that her team sees them on a frequent basis. “However, when our patients are on oral chemo, we feel that TapCloud is especially valuable to give us a window into their experience. We risk losing them because they cannot tolerate the medications and stop without communicating to us.”
- Address Patient Needs with Right Resource: When patients are not in the Clinic or Hospital, it is important to understand what they need. “We may see in a patient’s journaling that she is feeling afraid which is not physical but may be best addressed through our psych- social resource. Or a patient may be ‘running out of her medication’ or ‘checking in on an upcoming appointment’, which can be managed by our Nurse Coordinator."
Measuring Success
Dr. Twaddle uses a set of quantitative and qualitative measures to evaluate the success for the TapCloud solution for oncology patients including:
1) Patient Engagement. How involved are patients in participating in their care? How often did they check in with the app? Which symptoms are most common? What are the new symptoms that have been added by the patient?
2) Improved symptom management. Was pain successfully controlled (e.g. pain scores, pain direction)? Were negative symptoms (e.g. fatigue, bloated, shoulder pain) managed in a timely and effective manner?
3) Cost reduction. How much money was saved by avoiding ER through interventions on symptoms? “When one of our cancer patient ends up in the ER, we explain that we may be able to help avoid the admission with a check in on the TapCloud tool. We had one patient with a side effect that we could have spotted and intervened since it was dangerous for her”.
“We have found that TapCloud is helpful both with cancer patients who have declining function (e.g. pancreatic, advanced lung, brain tumor) and with those that may be curable (e.g. head & neck, breast)", shares Dr. Twaddle.
AMITA Health’s Program will leverage TapCloud
AMITA Health, one of Illinois’s largest health systems is in the process of planning their program which will use TapCloud.
“When I first heard about TapCloud, I was on board immediately”, explains Dr. Robert O. Maganini, Breast Cancer Specialist at AMITA Health. “We have a compliance problem with our breast cancer patients. Although the hormone therapy treatment (e.g. Tamoxifen, Class Aromatase inhibitor) is for five years, some patients will stop after two years because of the side effects. Our working theory is if we have insights into where these patients struggle and when, we can do more aggressive interventions instead of waiting for their next appointment”.
“Our plan is to offer TapCloud to all 200 patients who want to use it, from newly diagnosed to those in year two when we experience a drop in treatment adherence”. After describing his patient population – mostly women 40-75 years old, Dr. Maganini expects a high opt- in rate since it is “ideal for them because it enables faster and more convenient access to their provider”.
Like Dr. Twaddle, Dr. Maganini is planning to use a patient- centric approach when introducing TapCloud, ensuring that patients understand why they are using TapCloud, how to use it, and when to use it.
Dr. Maganini plans to introduce TapCloud to patients at the time of diagnosis. Nurses (e.g. NPs, Navigators) will get patients set up and show them how to use the digital health application. “Since surgery is typically the first step, we plan to use as a follow up with discharge instructions. For those in going through chemo treatments, we will monitor their symptoms. We want to get our patients accustomed to using TapCloud and then they will be using it for the long run with hormone therapy”.
As part of the planning process, Dr. Maganini is working with his team to define the list of side effects including the words that these patients use to describe them. He is leveraging his own and his nursing staff’s patient experiences to devise the TapCloud symptom list in “patient speak”. This is helpful to patients who often struggle to describe their symptoms and feelings.
From this program, Dr. Managini expects to learn about the top side effects, interventions and the effectiveness of the interventions. He will be looking at different success factors – “increase in the therapy completion (3, 4, 5 years) and longer term (beyond the 2 years) hopefully a decrease in mortality rate and reoccurrence”.
“With a program showing demonstrative effectiveness, we envision scaling this to the AMITA Health 2.0, 19 hospitals”, concludes Dr. Managini.
 Permalink
Permalink  consumer generated health and wellness content,
consumer generated health and wellness content,  mobile health and wellness texting,
mobile health and wellness texting,  patient education,
patient education,  patient engagement,
patient engagement,  patient experience,
patient experience,  patient journey,
patient journey,  patient reported experience measures,
patient reported experience measures,  patient reported outcome measures,
patient reported outcome measures,  personalization for health and wellness in
personalization for health and wellness in  AI consumer engagement,
AI consumer engagement,  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care collaboration,
Care collaboration,  Caregiver digital health,
Caregiver digital health,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  Population Health,
Population Health,  TeleHealth,
TeleHealth,  TeleMedicine,
TeleMedicine,  patient health education,
patient health education,  shared decision making ehealth
shared decision making ehealth Northwell Health’s Patients engage with AI ChatBot for guidance & support through their care journey
 November 6, 2018
November 6, 2018 Northwell Health, New York’s large integrated health system with 22 hospitals and 550+ outpatient facilities, recognizes the importance of leveraging technology to extend the care team and personalize the patient journey.
With the launch Northwell Health Chats (powered by Conversa Health), patients are empowered to connect, communicate and collaborate with their care team, while their clinicians closely monitor the patient’s evolving needs.
 Think about a patient’s journey today. Pamela, a 78 year old Medicare patient has just been discharged from a Northwell Hospital for a heart failure episode.
Think about a patient’s journey today. Pamela, a 78 year old Medicare patient has just been discharged from a Northwell Hospital for a heart failure episode.
Fortunately for Pamela, Northwell’s Health Chats, a new conversational AI platform will help support her during her recovery. With this text based chatbot, Pamela receives many more outreaches from her care team, a three- fold increase from about five times to fifteen during the 30 days post discharge period.
When she returns home, Pamela starts receiving notifications through SMS text message and clicks on the link to begin her chat about how she is doing. These chats continue to support Pamela through her recovery.
Pamela is asked to confirm her weight uploaded automatically from her Withings scale. She sees her weight trending map with an educational message about working towards her goal. Next, Pamela responds how she is doing with her leg swelling and then about any difficulty breathing.
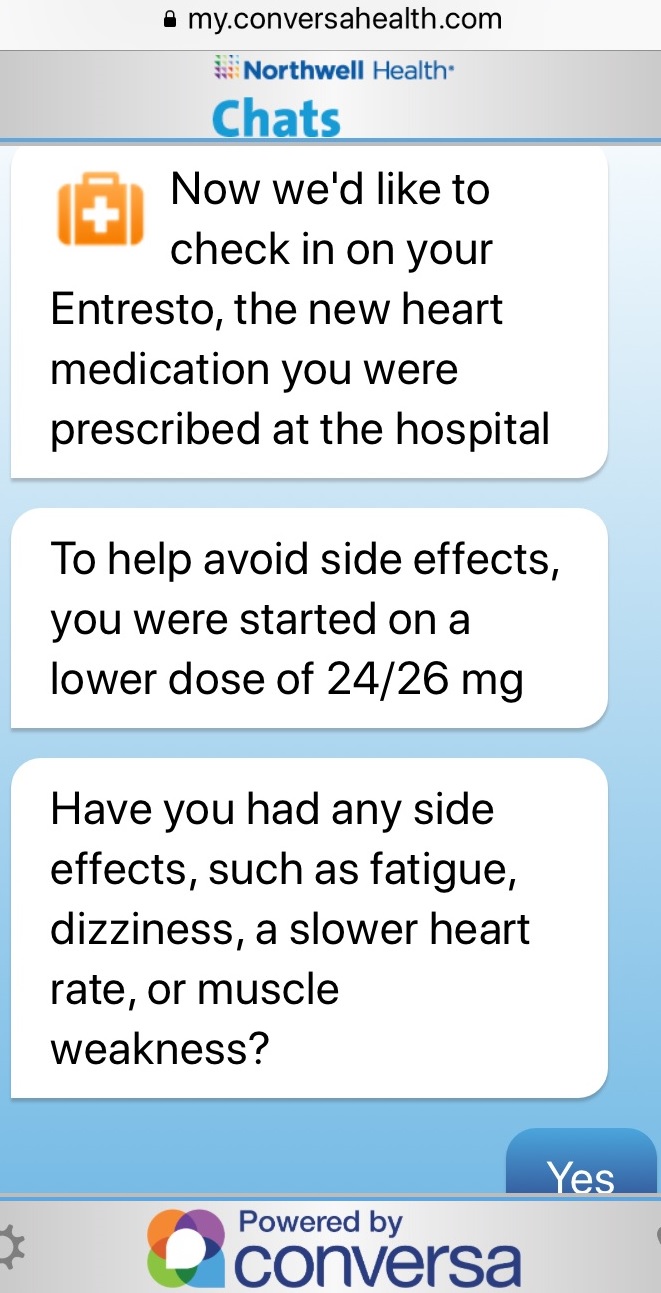 Finally, the chat asks Pamela to indicate any side effects of her new medication. Based on her responses, she may be connected with her nurse to discuss any medication adjustments. All of the information that Pamela provided to the chatbot is shared with her nurse for their discussion.
Finally, the chat asks Pamela to indicate any side effects of her new medication. Based on her responses, she may be connected with her nurse to discuss any medication adjustments. All of the information that Pamela provided to the chatbot is shared with her nurse for their discussion.
Since this patient engagement solution is seamlessly integrated into Northwell’s work flow (e.g. care management tool/HIE), Pamela receives these personalized chats from her specific Nurse Navigator at Northwell and the chat content is tailored for her specific care journey. Pamela trusts the information that she receives and can respond with questions and concerns at any time. Pamela’s Nurse Navigator will determine if she needs to come right in to the office or if they can address her issues through a text, email, call or telehealth visit.
Northwell is leveraging their Health Chats for population health. For example, the chat support patients as they prepare for a colonoscopy in their own language, ensuring the patient understands the instructions and knows how important this screening is to their health. This chat helps increase the patient’s health literacy and confirms that the patient knows how to prepare, reducing delays in diagnosis and additional health costs.
Positive Results with Northwell Health Chats
Sabina Zak, VP Northwell Community Health believes this chatbot is a “way to engage patients, by embedding information that is accurate, actionable and enables them to make more informed decisions which leads to better outcomes”.
As Northwell rolls out their Health Chats across the enterprise, they will be monitoring care quality, care cost and patient satisfaction measures. With Northwell Health Chats, they are seeing a 97% patient satisfaction rate and lower post-acute care expenses in some of its hospitals. Northwell management is particularity interested in the reduced costs from fewer outreach calls since the bot engages patients and brings back needed information.
Patient Comment:
“These conversations were great and supportive emotionally as well as medically”.
Nurse Leader Comment:
“Conversa gives me reassurance that my patients are ok because I can see that they are responding to the health chats. It gives me piece of mind knowing that they are alright without having to always call them.”
Clinical Leader Comment:
“Innovative technologies like Northwell Health Chats are critical assets in our journey towards providing excellent clinical care and an outstanding personalized patient experience”, explains Northwell Health physician Dr. Zenobia Brown, VP Population Health.
Expanding Conversational Chat at Northwell Health
In addition to supporting patients through procedures such as Colonoscopies, Northwell will be using this conversational chatbot to gather social determinants of health before the patient’s annual office visit. This information will be shared with their care team for their appointment.
Beyond population health, Northwell is expanding their Health Chats into Oncology, starting with head and neck and expanding to breast and prostate cancer patients. Northwell’s Health Chats will help patients prepare for the treatment, manage symptoms and check in once the treatment has concluded.
In the future, Northwell is planning to use their Health Chats in the areas of bundled payments for patients with Coronary Artery bypass, Acute MI, Pneumonia, Stroke and Heart Failure.
“Conversa’s conversational AI powering Northwell Health Chats enables us to improve care coordination, patient satisfaction and our ongoing patient relationship, resulting in the improved well-being of our customers while reducing costs. This high-tech, high touch, scalable approach benefits our patients, our nurses and our health system”, concludes Joseph Schulman, SVP Regional Executive Director at Northwell Health.
 Motivation for health and wellness,
Motivation for health and wellness,  educating consumers about health and wellness,
educating consumers about health and wellness,  online health and wellness coaching,
online health and wellness coaching,  patient education,
patient education,  patient experience,
patient experience,  patient journey,
patient journey,  personalization for health and wellness in
personalization for health and wellness in  AI consumer engagement,
AI consumer engagement,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  patient health education
patient health education Dartmouth- Hitchcock’s ImagineCare Platform Leverages Wearables, Connected Health & Analytics for Personalized Patient Care
 October 16, 2016
October 16, 2016  Dartmouth-Hitchcock (D-H), an innovative New England healthcare system with 1,000+ providers is committed to creating a “sustainable health system”, which proactively engages patients through new care models to achieve the triple aim.
Dartmouth-Hitchcock (D-H), an innovative New England healthcare system with 1,000+ providers is committed to creating a “sustainable health system”, which proactively engages patients through new care models to achieve the triple aim.
Over the years, D-H has invested in technologies that empower patients to collaborate with providers through shared decision tools and Telehealth, treating “patients and their families as partners in care”.
D-H has been a pioneer in innovative payment models with both the government and commercial payers.
In early 2015, D-H’s leadership team committed to create a truly patient-centric healthcare organization, which delivers high quality proactive personalized care to the patient beyond the hospital walls.
“Dartmouth-Hitchcock purposefully set out to assemble a team of employees with backgrounds from other consumer industries like hospitality and retail that would augment the world-class capabilities of our clinical staff, to improve the health care delivery experience”, explains Vin Fusca, COO, ImagineCare.
With their consumer- centric “healthcare without boundaries” vision, D-H management has designed a truly “care- driven” solution. ImagineCare, a cloud- based platform, enables providers to closely collaborate with each patient to meet her care goals at any time and from anywhere.
ImagineCare treats the patient holistically through the active and passive collection of a comprehensive set of patient data. In addition to condition specific evidence-based care pathways (i.e. ImagineCare Hypertension Pathway, COPD Pathway, CHF Pathway, Diabetes Pathway), D-H incorporates a “Core Health Pathway” to capture steps, heart-rate activity, sleep, and stress (Behavioral Health), providing contextual insight into the patient’s health.
With ImagineCare, the Provider and patient have a window into the latest health status for insight and action. In the background, ImagineCare collects information from the patient (i.e. sensor- based devices, apps), combines it with EMR data (i.e. patient visits, labs, meds) and processes it through complex clinical care algorithms with machine intelligence to pinpoint when the patient is at risk. High tech meets high touch when ImagineCare notifies the RN or Health Navigator to reach out to the patient for real-time support and intervention.
 “ImagineCare leverages the best available technologies to assist with care, but does not replace the importance of the human touch to drive behavior change. ImagineCare seamlessly combines these components to help patients achieve their health goals”, shares Dr. Ethan Berke, Chief Medical Officer, ImagineCare.
“ImagineCare leverages the best available technologies to assist with care, but does not replace the importance of the human touch to drive behavior change. ImagineCare seamlessly combines these components to help patients achieve their health goals”, shares Dr. Ethan Berke, Chief Medical Officer, ImagineCare.
Patient Experience
During her recent doctor’s visit, (patient) Pam decides to participate in D-H’s new ImagineCare Program to help her lose weight and proactively manage her hypertension.
Within 48 hours, Pam receives an email to quickly enroll in ImagineCare and a welcome call to discuss her personal health goals. Two days later a personalized ImagineCare Kit (box) is delivered to her door containing a program overview, a wireless blood pressure cuff and an activity band, devices which fit her selected health goals. Pam follows the instructions to connect her devices to the ImagineCare app.
During enrollment, Pam’s shares her profile information such as personal health goals, challenges, communication preferences, family support, and defines her “medical neighborhood” (i.e. Providers, pharmacy, caregivers). She adds more information when responding to daily questions to create a rich picture about her health needs and resources required to tackle care plan activities.
Anxious about her attempts to lose weight, Pam indicates in the mobile app that she only wants to receive texts to help her stay on track with her weight-management goal.
Through the ImagineCare mobile app, Pam answers daily questions about how she is really doing, while her wireless blood pressure cuff and activity band retrieve and send real-time measures. Pam receives nudges, encouraging messages and digital check-ins to ensure she stays on track with her care plan. Yesterday’s text asked Pam if she was okay since she hadn’t provided her blood pressure as expected.
D-H’s RNs and Health Navigators continuously monitor Pam’s health status, review her trends, and respond to risk warnings by reaching out via text which is her communication preference. Since Pam designates her daughter as a personal health representative within the mobile app, ImagineCare’s RNs are permitted to speak with her about Pam’s health.
ImagineCare Success Measurement
ImagineCare is designed to empower a health care organization to right-size provider visits, lower ED utilization and decrease admission and re-admissions. ImagineCare provides a more engaging solution to help health care delivery systems increase quality of care, decrease cost and improve patient experience.
In addition to these quantitative measures, D-H actively gathers qualitative patient feedback to understand the patient experience. Comments from patients about engaging in the ImagineCare program include:
“I monitor my blood pressure every day, and after a particularly stressful day at the office I went home, took my blood pressure, and five minutes later one of the nurses called and talked me through an immediate care protocol.”
“It has improved my ability to manage my health…The ability to connect with people for support and also send information to my healthcare providers, makes it easier.”
"I am extremely impressed with the ImagineCare phone app. It is very easy to use and seems very intuitive”.
ImagineCare Future
ImagineCare is constantly updating its services and products based on patience engagement data, clinical data, and new technological capabilities coming to market. In a digital health landscape that is becoming more fragmented, ImagineCare will continually create holistic, customer-centered health services to better care for patient populations.
D-H’s team has packaged up the ImagineCare platform for other providers, payers and (self- insured) employers to deliver personalized patient care for better outcomes.
 consumer generated health and wellness content,
consumer generated health and wellness content,  mobile health and wellness texting,
mobile health and wellness texting,  online health and wellness support,
online health and wellness support,  personalization for health and wellness,
personalization for health and wellness,  wearables health in
wearables health in  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  TeleHealth,
TeleHealth,  shared decision making ehealth
shared decision making ehealth Virtua Navigates Orthopedic Patients Pre- & Post-Surgery with Improved Patient Engagement and Care Coordination
 May 19, 2016
May 19, 2016 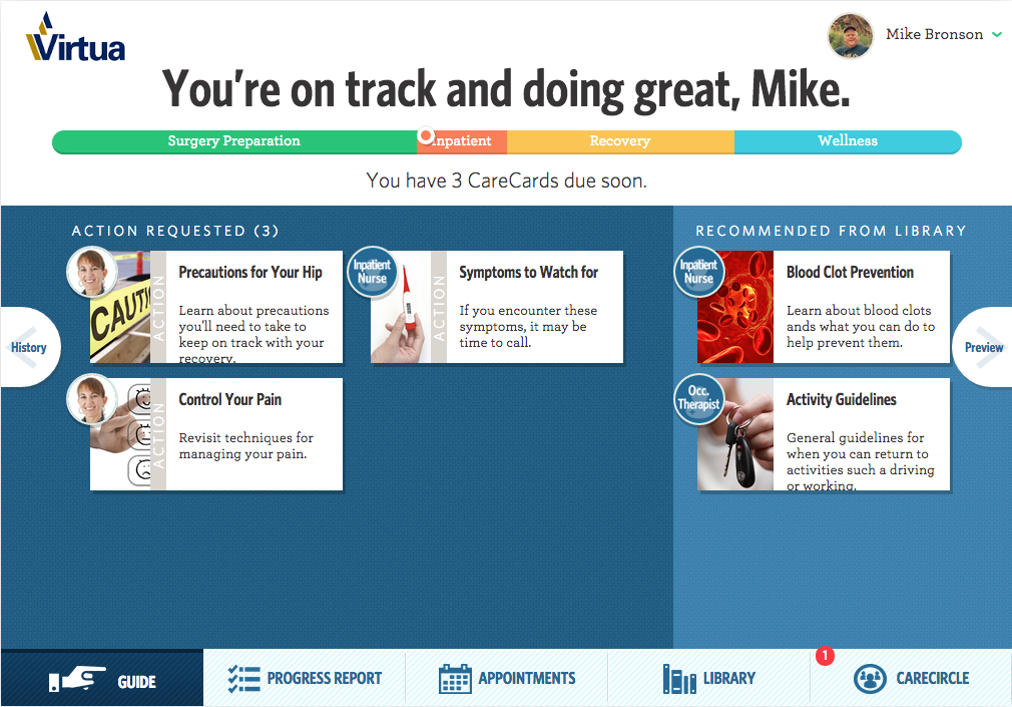 WELLBE PLATFORM FOR PATIENT ENGAGEMENTWith an aging population and increase in chronic conditions including obesity, the demand for hip and knee operation is increasing dramatically. A study in the Journal of Bone & Joint Surgery estimates by 2030 “demand for total hip arthroplasties to grow by 174% to 572,000 and demand for primary total knee arthroplasties by 673% to 3.48 million procedures”.
WELLBE PLATFORM FOR PATIENT ENGAGEMENTWith an aging population and increase in chronic conditions including obesity, the demand for hip and knee operation is increasing dramatically. A study in the Journal of Bone & Joint Surgery estimates by 2030 “demand for total hip arthroplasties to grow by 174% to 572,000 and demand for primary total knee arthroplasties by 673% to 3.48 million procedures”.
 PATIENT CREATES CARECIRCLE ON WELLBEDuring the initial visit to the surgeon’s office, patient Patty is given information about Wellbe, a personalized care plan for her pre-and post-surgical journey. She signs up with the Nurse Navigator and receives a Welcome email. Patty shares this information and invites her family ‘Care Partner’ to join her CareCircle to access her resources.
PATIENT CREATES CARECIRCLE ON WELLBEDuring the initial visit to the surgeon’s office, patient Patty is given information about Wellbe, a personalized care plan for her pre-and post-surgical journey. She signs up with the Nurse Navigator and receives a Welcome email. Patty shares this information and invites her family ‘Care Partner’ to join her CareCircle to access her resources.
 Motivation for health and wellness,
Motivation for health and wellness,  consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  online health and wellness support,
online health and wellness support,  patient education,
patient education,  patient generated health data,
patient generated health data,  personalization for health and wellness in
personalization for health and wellness in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Care collaboration,
Care collaboration,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Patient Portal
Patient Portal