Healthloop Virtual Patient Check in
Healthloop Virtual Patient Check in
Healthcare reform has placed increased demands on doctors who are already managing increased patient loads. As a result, doctors are spending less time with their patients.
Patients are being asked to take on more responsibility in managing their care. This is particularly challenging before and after a surgical procedure. A patient typically leaves the hospital with a stack of paper discharge instructions about medications, the follow- up visit and a list of symptoms to monitor with directions to contact the doctor if problems occur. Throughout recovery, the patient is often left to figure things out because she "doesn’t want to bother the doctor". When the patient makes uninformed decisions about medications or readiness to begin an activity level, it can set her back on her recovery path or lead to costly hospital readmissions.
Other than checking in with patients during the follow- up visit, providers are in reactive mode; patients calling with complex problems or heading to the ER.
Since patient satisfaction, care quality and costs are impacted by the current process, providers are motivated to find a solution that virtually supports the patient's needs for guidance, education and shared decision making.
Virtual Patient Support
It all started in 2007 when Dr. Jordan Shlain was treating a patient who wasn’t feeling well. After discussing her symptoms, he gave the patient his cell number and asked to please call him if she felt worse by morning. He discovered a few days later that she had developed pneumonia. From this experience, Dr. Shlain learned that although he wanted to be proactive with his care, he couldn’t depend on the patient to call with an update. His began texting patients asking “do you feel the same, better or worse?” Dr. Shlain did not take any chances and assumed that a non- response from the patient indicated there may be a problem.
After speaking with providers about not really knowing how a patient is doing post discharge, they expressed interest in daily virtual interactions with the patient as a way to increase patient engagement and prevent readmissions. Patients loved the idea of interacting electronically with their doctor on a daily basis since it would give them unprecedented access to communicate concerns and address problems in a quick and convenient way. This was the backdrop that led to the development of Healthloop.
“Since late June, we have been using Healthloop for patients who have hip and knee replacement surgery”, shares Dr. Mohan, Surgeon for a large Integrated Delivery Network. “Our team was looking for a solution that would enable us to share the experience together with our patient. We also wanted to put the patient in the driver’s seat and give them control, while we were in the passenger seat as an observer and navigator.” Dr. Mohan’s orthopedic patients are on Healthloop before surgery and throughout recovery which tends to be 1-3 months.
Dr. Andrew Goldstone, ENT Surgeon at Greater Baltimore Medical Center started using Healthloop in February with his adult and pediatric patients throughout recovery which typically lasts 2-4 weeks. Healthloop electronic communications are delivered to the parents of his young patients for ongoing support. "HealthLoop, in a technologically modern way, tries to mimic the old days when we admitted patients a day or so before and kept them as many days as we or they wanted to stay after surgery. This gave patients and their families a comfort level that most current M.D.s have never witnessed. The same goes with patients who, after ambulatory surgery, pay at the next window and go home. They have no clue how patient friendly it used to be having an extended ’hand holding‘ before returning home. I view HealthLoop as an attempt to recreate that extended comfort,” explains Dr. Goldstone.
Patient Experience
HealthLoop enables the physician to support the patient before surgery and monitor him post discharge and between visits, engaging each patient “as if he is the most important person”. With the goal of delivering guidance when the patient needs it, Healthloop works closely with the provider organization to define the questions that patients ask at each step of the recovery process. Together, they review typical calls at day 1, 2, etc., determine the appropriate response and set up the schedule to deliver the information to the patient right when they need it.
Taking a closer look at the patient experience, Gary is referred by his primary care physician to a specialist about knee surgery. After deciding together to move forward with the operation, the surgeon quickly enrolls Gary in Healthloop to guide him before and after the surgery. Gary receives an email to complete his enrollment including his preferences for receiving Healthloop communications (i.e. email, text).
Before surgery, Gary answers questions about risk factors and receives guidance and checklists to prepare for his operation. For example, he learns how to to prepare his house to easily navigate when he returns home following surgery.
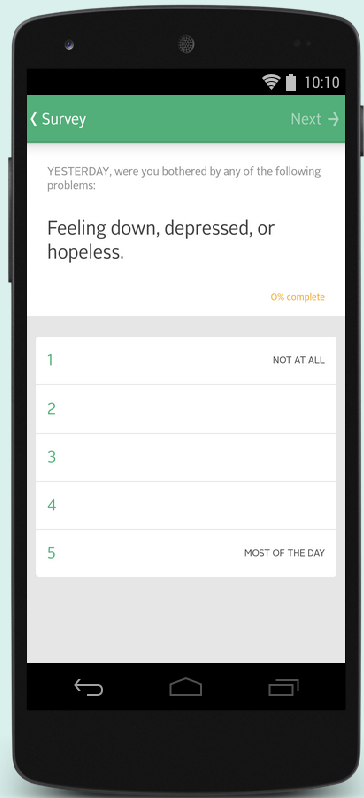
After surgery, Gary receives a daily electronic communication with a set of questions to understand how he is feeling (i.e. pain level, specific symptoms, problems with meds, etc.), personalized education materials, activity and medication reminders and a checklist of To Dos. Based on Gary’s feedback and progress, his care plan is updated and his next day’s check-in is automatically prepared.
Healthloop is designed for two way engagement. If Gary experiences any health problems, these are gathered through his check- in responses and trigger an SMS message to his care team for intervention and support.
With recent integration to Apple’s Healthkit, patient information is extended beyond daily check- in responses to include health tracking data. For example, Gary’s doctor has instructed him to take steps while healing from his knee operation. Gary’s tracker information is combined with his daily check-ins to give his care team more insight into his health status. Concerned about not enough movement, his clinician may call and learn that Gary is not moving enough because of his medication side effects which can be addressed through a prescription change.
Pilot Feedback; Patients & Providers
Healthloop wants to deliver a truly patient- centric communication channel and uses patient feedback to enhance the solution. After hearing a patient comment that the messages felt “too robotic” and “do not sound like they are coming from my doctor”, the communications were refined to be more conversational.
Another patient commented that the messages were using doctor’s words which resulted in changes to incorporate more patient vocabulary and experience. For example, questions about a blood clot were replaced with “feels like a cramp in my calf”.
Patient Comments
Healthloop has delivered over 57,000 daily check-ins to patients and has received positive feedback about the experience:
Guidance: “I wanted to be able to say ‘I have this” and have someone come back and say that is normal and here is the process. Then all of my negative energy goes away”, “easy way for me to make sure that I was on the track with my recovery”. “The questions promoted me to be more aware of my situation”.
Convenience: “Without Healthloop. I would have called (doctor) 5- 7 times”, “This saved me a trip to my doctor”.
Access: “It was an extension of my doctor so instead of talking to a nurse and having her get back to me, I had a direct conduit to my doctor.”
Provider Comments
 Healthloop Clinician Dashboard
Healthloop Clinician Dashboard
“As our team developed our Healthloop, we charted out what a recovery really is. With this, I know what my patient is going through, can emphasize and say with confidence that over half of my patients have their pain under control after day 4”, explains Dr. Mohan. “We also participate in a Medical Destination Program with patients traveling to our hospital, often from out of state. After staying in a hotel for 10- 14 days, they come to see me for a follow-up visit before returning home. We are now thinking about how we can use Healthloop to manage their care from a distance to make sure that the patient has a successful recovery.”
Comments from other providers:
Patient Satisfaction: “My patients told me that they looked forward to their daily Healthloop check-ins because it felt like ‘someone was watching over me’ who really cared”.
Operational Efficiency: “For my practice, the volume of calls from patients has dropped tremendously. I notice it and my staff notices it too.” “I am thinking about eliminating the 2 week follow-up visit and to just see the patient at the 6 week visit since I can check in on their pain management, incision and any other issues through Healthloop.”
Better Quality: “Helps us pick up complications much sooner. It reinforces a plan with what to do and reminders”, “We are raising the bar on care by ensuring that we are giving the patient the pre and post-surgery education and care that they need”.
Success Measures
Providers using Healthloop are evaluating a set of success factors based on their program goals. In addition to lower costs which is measured over time, providers are monitoring:
Patient Engagement; Patient Satisfaction using the net promoter score.
Better Quality; Benchmarking patient progress, measuring patient’s perceptions of care quality received
Operational Efficiency; Call reduction to the practice
Regarding patient engagement, some providers are leveraging positive ratings through social media. Patients who give the highest scores (5 Star Ratings) are encouraged to share their ratings and experiences through the link provided to public review sites such as HealthGrades and Vitals. Patients who give average or below average score are asked to explain how the provider can improve. Patients have commented on everything from old waiting room magazines to being put on hold for too long when they call.
With Healthloop, “my patients tell me that they are happy with the surgery because I was right there with them. I also notice patients are much more relaxed during their follow-up appointments. That is so important to me”, Dr. Mohan concludes.
 consumer generated health and wellness content,
consumer generated health and wellness content,  educating consumers about health and wellness,
educating consumers about health and wellness,  mobile health and wellness texting,
mobile health and wellness texting,  mobile health application,
mobile health application,  online health and wellness support,
online health and wellness support,  patient ehealth engagement,
patient ehealth engagement,  self- management health tools in
self- management health tools in  Behavior Change Health & Wellness,
Behavior Change Health & Wellness,  Connected Health,
Connected Health,  Data Driven Health Engagement,
Data Driven Health Engagement,  Decision Support eHealth,
Decision Support eHealth,  Mobile Engagement Health & Wellness,
Mobile Engagement Health & Wellness,  Patient Decision Support,
Patient Decision Support,  Patient Engagement,
Patient Engagement,  Personalization eHealth,
Personalization eHealth,  Population health management,
Population health management,  TeleHealth,
TeleHealth,  shared decision making ehealth
shared decision making ehealth