During the World Congress Patient Experience & Engagement Summit in Boston, I led a panel with these innovative health systems, discussing how they are using virtual health assistants (e.g. AI Chatbots, Voice) to increase efficiency in care delivery and enhance the patient experience.
During the World Congress Patient Experience & Engagement Summit in Boston, I led a panel with these innovative health systems, discussing how they are using virtual health assistants (e.g. AI Chatbots, Voice) to increase efficiency in care delivery and enhance the patient experience.
Virtual Assistants in Healthcare
Consumers are demanding convenience and want to interact with companies any time anywhere. Companies across different industries such as retail, travel and financial services are responding with virtual assistant tools, enabling consumers to get answers and transact 24x7.
Within healthcare, innovation driven organizations are exploring how to empower patients with virtual health agents to access relevant care information (e.g. learn about how to prepare for a procedure, determine when to call the doctor following surgery), get tasks done (e.g. schedule and participate in a virtual visit) and get guidance on a care plan (e.g. reminders to refill medication, follow up doctor’s appointments).
The strong interest in AI driven virtual health assistants aligns with Accenture’s Digital Health Tech Vision 2019 trend #5 “MYMARKETS: Meeting customer’s needs at the speed of now”. The Accenture report explains “digital expectations have now evolved and a new opportunity to deliver better experiences is on the table: capturing moments. Technology has created a world of intensely customized and on-demand experiences, so healthcare organizations must reinvent themselves to find and capture those opportunities as they come”.
Value of Virtual Health Assistants
When you think about the gaps in healthcare efficiency today, you can envision how virtual health assistants can support patients and the care team.
There are many valuable use cases for Virtual Health Assistants to help patients prepare and manage their care, with reminders, education (e.g. health condition, procedure) and the capability to escalate to a care provider as needed.
On the clinical side, the care team can capture, monitor and communicate with patients. Instead of making outbound calls trying to reach patients, staff can see which patients are in pain, have questions/concerns or are in need of immediate care.
Panelist Virtual Health Assistant Use Cases
When presenting their use cases for Virtual Health Assistants, panelists shared their specific business goals such as decreasing readmissions/ED visits and costs, increasing service utilization, improving care plan compliance and enhancing the patient experience. All panelists view these virtual health assistants as an “extension” of their care delivery.
 Boston Children’s Hospital (BCH): In 2018, BCH teamed up with Seattle Children’s on an Alexa skill, Flu Doctor, providing parents with answers to questions about the flu which are “personalized, science-backed data and recommendations”. Panelist Devin Nadar, Senior Partnerships Manager, Innovation and Digital Health Accelerator discussed a more recent Alexa skill -“My Children’s Enhanced Recovery After Surgery (ERAS)”, which is part of the program for all cardiac patients undergoing specific surgeries at BCH. Built on the Amazon platform, this skill to desgned to capture information from the parent about how the child is doing after the surgery and indicate if there is a follow up appointment scheduled. “We know that parents really don’t want to come back to the hospital after surgery”, Devin adds. After accessing “My Childrens” through the Amazon Alexa Store, the parent begins to “check in” the day after the patient is discharged and receives pertinent information for that day.” Before this tool, it was “like a black box” about what happens while the patient is recovering. Now BCH can focus clinical resources on patients with priority needs.
Boston Children’s Hospital (BCH): In 2018, BCH teamed up with Seattle Children’s on an Alexa skill, Flu Doctor, providing parents with answers to questions about the flu which are “personalized, science-backed data and recommendations”. Panelist Devin Nadar, Senior Partnerships Manager, Innovation and Digital Health Accelerator discussed a more recent Alexa skill -“My Children’s Enhanced Recovery After Surgery (ERAS)”, which is part of the program for all cardiac patients undergoing specific surgeries at BCH. Built on the Amazon platform, this skill to desgned to capture information from the parent about how the child is doing after the surgery and indicate if there is a follow up appointment scheduled. “We know that parents really don’t want to come back to the hospital after surgery”, Devin adds. After accessing “My Childrens” through the Amazon Alexa Store, the parent begins to “check in” the day after the patient is discharged and receives pertinent information for that day.” Before this tool, it was “like a black box” about what happens while the patient is recovering. Now BCH can focus clinical resources on patients with priority needs.
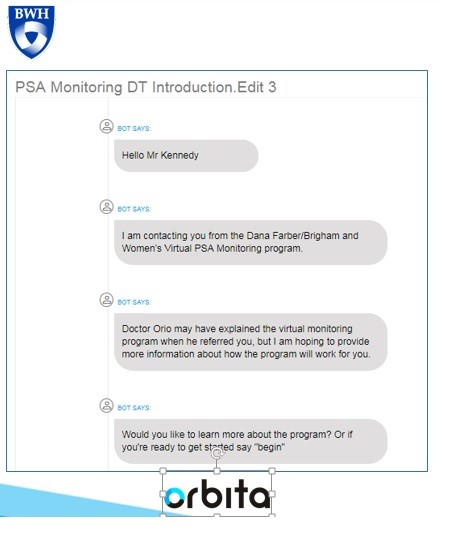 Dana-Farber/Brigham and Women's Cancer: “Earlier this year we developed and are planning to launch an Orbita powered health assistant to support prostate cancer patients who are on a “lifelong journey” with ongoing PSA testing” shares Rich Boyajian, NP Program Director, Virtual PSA Monitoring, Radiation Oncology. This chatbot will send a link to the patient to engage via text and/or voice on their phone. It is designed to “onboard” him into the program, present the closest lab, deliver good PSA test results and enable him to request contact with a care team member. “Patients can select the modality for this follow up contact by email, a call or even a virtual visit”, explains Rich. “It was easy for me to write the virtual health assistant script (i.e. questions and answers) to engage with the patient since I do this all the time. We selected the Orbita platform because we can put this content in one time and it be accessed by the patient through their preferred modality”.
Dana-Farber/Brigham and Women's Cancer: “Earlier this year we developed and are planning to launch an Orbita powered health assistant to support prostate cancer patients who are on a “lifelong journey” with ongoing PSA testing” shares Rich Boyajian, NP Program Director, Virtual PSA Monitoring, Radiation Oncology. This chatbot will send a link to the patient to engage via text and/or voice on their phone. It is designed to “onboard” him into the program, present the closest lab, deliver good PSA test results and enable him to request contact with a care team member. “Patients can select the modality for this follow up contact by email, a call or even a virtual visit”, explains Rich. “It was easy for me to write the virtual health assistant script (i.e. questions and answers) to engage with the patient since I do this all the time. We selected the Orbita platform because we can put this content in one time and it be accessed by the patient through their preferred modality”.
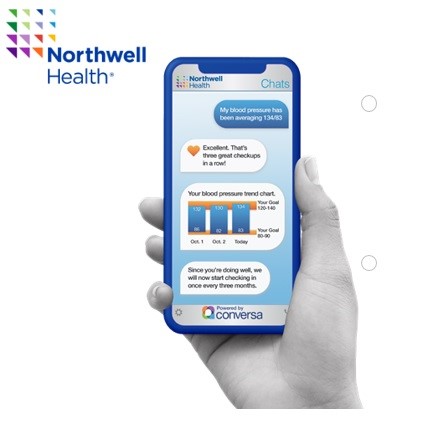
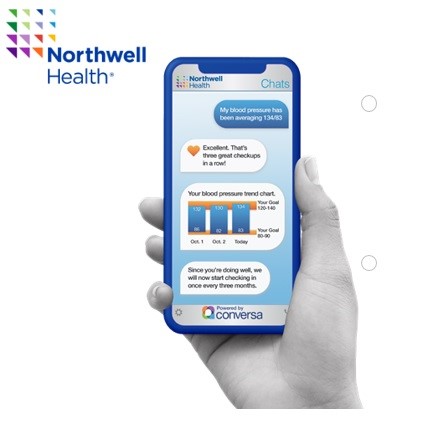 Northwell Health: In 2018, Northwell launched Health Chats, an AI text chatbot powered by Conversa Health, which empowers patients to stay connected to their care navigator through recovery. This gives the staff visibility into what is really happening when the patient leaves the hospital. “We selected Conversa Health because it is easy for the patient who doesn’t need to download an app. Instead the patient receives a chat notification through an email or SMS text message and simply clicks on the link to start the chat through their mobile phone”, explains Hallie Bleau, ACNP-BC, AVP Transitional Care Management, Health Solutions. The Health Chat engages the patient post discharge to “self -assess and manage symptoms”. Since Northwell Health integrated the Health Chat into their care management system, the information that the patient types in (problems, pain level) is feed into an algorithm to flag the patient on the nurse’s dashboard for an immediate contact. The patient can connect with a nurse through the Health Chat application at any time.
Northwell Health: In 2018, Northwell launched Health Chats, an AI text chatbot powered by Conversa Health, which empowers patients to stay connected to their care navigator through recovery. This gives the staff visibility into what is really happening when the patient leaves the hospital. “We selected Conversa Health because it is easy for the patient who doesn’t need to download an app. Instead the patient receives a chat notification through an email or SMS text message and simply clicks on the link to start the chat through their mobile phone”, explains Hallie Bleau, ACNP-BC, AVP Transitional Care Management, Health Solutions. The Health Chat engages the patient post discharge to “self -assess and manage symptoms”. Since Northwell Health integrated the Health Chat into their care management system, the information that the patient types in (problems, pain level) is feed into an algorithm to flag the patient on the nurse’s dashboard for an immediate contact. The patient can connect with a nurse through the Health Chat application at any time.
Panelist Insights on Virtual Health Assistants
Many lessons learned were shared by the panelists including considerations for both patient and staff engagement. One common theme was that the planning for these Virtual Health Assistants takes time. “We needed 6-8 months to get staff buy- in and patient consent”, admits Hallie.
Patient Considerations:
Determine fit with the patient’s current technology. “With our 65+ Medicare population at Northwell Health, we realized that one big barrier was some patients still have a flip phone which will not work with our chatbot”, Hallie explains.
Understand patient expectations. “In our Alexa skill, we ask if the caregiver would like the doctor/nurse to call. We know there are differences in how long the call back will take so we need to set the proper expectations for when they can expect a return call ”, shares Devin.
All panelists expressed an interest in learning from patients about their experiences. “We built into the Alexa skill ‘did that answer your question’ so that we can capture their feedback and make changes to our script”, Devin explains.
Patients have shared insightful comments about their virtual health assistant interactions. “Our patients at Northwell Health feel that someone is always thinking about them. In a 30 day period, we are able to increase the number of touches by 5-6 contacts”. Hallie went on to say “we thought that caregivers would be more interested in seeing these digital conversations with mom. We learned some didn’t because ‘she doesn’t live with me’. Several seniors do not want to ‘bother their daughter with this information’. We have also learned that patients who are hard of hearing really like to use the chatbot because it is easier to communicate with the care team”.
Staff Considerations:
During the planning stages, panelists feel it is important to educate their staff. They need to feel comfortable with this new digital interaction, understand how to describe it to patients and have a clear picture how this will impact their workflow. Specific considerations include:
Extensive staff education. “We were surprised at the amount of time/education required with our staff. They needed to understand why and what does it mean for them”, admits Hallie.
Devin adds “we train with our staff, demonstrate the app and provide a cheat sheet for reference, which tells about them about our Alexa skill, how to open it, start it, stop it, what you can ask and what it is used for”.
Stage the implementation. “We have limited the roll out of the voice app to 5-10 per week because we did not want to overwhelm our staff at BCH”, explains Devin.
Success Measures & Future Virtual Health Assistants
Later in the year, panelists will be evaluating their program from an experience (patient, staff), operational efficiency and clinical perspective.
“At BCH, we want to see if parents are completing the questions and determining where they drop off so that we can build a better experience”, describes Devin.
“Our virtual health assistant is replacing the manual labor from looking up the nearest lab to calling cancer patients about positive test results”, shares Rich. “As an extension of our care, we expect to decrease the number of follow up in person visits which will free us up to care for more patients”.
“Our staff is seeing the fruits of labor… ‘we don’t have to call him’, ‘we can quickly get to the root of the problem”, adds Hallie.
Panelists expressed the need in the future to capture and place pertinent information from the digital health interaction into the patient’s electronic medical record.
Future Plans:
Refine conversation based on role. “At Northwell Health, we are talking about tweaking the conversation for the caregiver”, explains Hallie.
Expand languages. “We currently offer our chatbot in English and Spanish but will add other languages”, Hallie shares.
Add new capabilities. “We plan to add more symptoms to our health assistant to provide more information for our PSA monitoring”, explains Rich.
Extend the Experience. “We are working on expanding the digital conversation from 30 to 90 days so that we have more insight into their receovery”, mentions Hallie.
Connect into Virtual Care. “At BCH, we are thinking about triggering a virtual visit when the parent indicates that she needs to speak with someone”, shares Devin.
Northwell Health is planning to continuously launch Health Chats across their organization given their strategic investment in ConversaHealth. “We have already launched Health Chats to patients with head and neck cancer and are getting ready to roll out them out in our cardiac surgery department” Hallie concludes.
 chatbot,
chatbot,  mobile health and wellness texting,
mobile health and wellness texting,  online health and wellness support,
online health and wellness support,  research on consumer health in
research on consumer health in  AI,
AI,  AI consumer engagement,
AI consumer engagement,  Decision support,
Decision support,  Mobile Health,
Mobile Health,  Patient Engagement,
Patient Engagement,  Patient Experience,
Patient Experience,  Patient Journey,
Patient Journey,  Personalization eHealth,
Personalization eHealth,  digital health,
digital health,  patient health education
patient health education